Research Article - Archives of Clinical and Experimental Surgery (2022)
A Comparative Study of One-stage, Two-stage and Three-stage Posterior Sagittal Anorectoplasty (PSARP) in Female Anorectal Malformations (ARM)
Ashok Laddha1, Brijesh Lahoti1, Maneesh Jholeya1, Aditi Deewan2*, Shashi Shankar Sharma1, Ram Mohan Shukla1, Pooja Tiwari1 and Yashaswi Choudhury22Department of General Surgery, M.G.M Medical College, Indore, India
Aditi Deewan, Department of General Surgery, M.G.M Medical College, Indore, India, Email: aditi04.diwan@gmail.com
Received: 18-Apr-2022, Manuscript No. EJMACES-22-63135; Editor assigned: 20-Apr-2022, Pre QC No. EJMACES-22-63135 (PQ); Reviewed: 05-May-2022, QC No. EJMACES-22-63135; Revised: 10-May-2022, Manuscript No. EJMACES-22-63135 (R); Published: 19-May-2022
Abstract
Context: PSARP has been the standard treatment for ARM since the 1980s. PSARP can be done as a single procedure or as a staged procedure (two-stage or three-stage). Two-stage PSARP is a relatively new concept where colostomy and PSARP are done in the same stage, followed by stoma closure as second stage. Two-stage PSARP is a resource effective method, with minimal incidences of wound complications in the management of female ARM.
Aim: To compare the short-term complications and resource-effectiveness of one- stage, two-stage and three-stage PSARP in female ARM.
Settings and design: A prospective comparative study design was used. Seventy-four females were included in the study and randomly assigned to one of three groups (Groups A, B, and C undergoing one-stage, two-stage, and three-stage surgery, respectively). Patients with common cloaca and the children who did not complete all the stages were excluded from the study.
Methods: Patient‘s demographic data, duration of surgeries, number of days of hospital stay and postoperative complications, including wound infection, dehiscence, anal stenosis and recurrence of fistula were noted. Student’s t test and Oneway ANOVA with post-hoc Tukey HSD Test were used to compare the postoperative complications.
Results: The wound complications were found to be higher in Group A (51.6%) when compared to group B (14.3%) and Group C (4.5%). (p=0.001), whereas the wound complication rates were similar in groups B and C. The total duration of hospital stay and total duration of surgery were the least in group A (7.52 ± 1.91 days) and highest in Group C (16.64 ± 5.76 days). Group B had significantly lesser operative time and total duration of hospital stay than Group C.
Conclusion: A colostomy has a protective effect in preventing wound complications. Both two-stage and three-stage PSARP have similar results in terms of complications and outcome. Two-stage surgery has the additional advantage of omission of one surgery and lesser duration of hospital stays and follows up.
Keywords
PSARP; Anorectal malformation; Female; Two-stage
Introduction
Anorectal Malformations (ARMs) comprise a wide spectrum of congenital anomalies involving the distal rectum and anus as well as the genital and urinary tracts, affecting both males and females with worldwide incidence of 1 in 5000 live births [1]. It is slightly more common in males than in females. Female ARM is “low” type 90 % of the time. The most common Anorectal anomaly in female newborns is Recto Vestibular Fistula (RVF), the next common anomaly being common cloaca, imperforate anus without fistula occurs in less than 5% of cases [2].
Since the 1980s, PSARP is considered the standard approach for definitive repair of ARM [3]. In female newborns with anomalies other than cloaca, reconstructive surgery can be performed as a single-stage or a multi- stage procedure with a diverting transverse or sigmoid colostomy. It is still under debate if a diverting colostomy provides any benefit when weighed against the potential complications of stoma.
Traditionally, three-stage repair was performed in all neonates with ARM, it had the disadvantage of three operations and high dropout rates after colostomy [4]. We proposed this study to assess and compare the efficacy of one-stage, two-stage and three-stage PSARP in terms of wound complications, complications of colostomy and cost and resource effectiveness.
Materials and Methods
The present study was conducted on female patients with ARM who presented from November 2020 to November 2021 and was treated by Posterior Sagittal route. A Prospective comparative study design was adopted. Male newborns with ARM, female newborns with common cloaca, pouch colon and patients who died before surgical correction (PSARP) or did not complete all stages of surgery, were excluded from the study.
A total of 78 patients were included in the study. The children who presented without any of life threatening associated congenital anomaly (especially cardiac) and with absence of gross abdominal distension, were randomly assigned to group A, B and C. Group A (31 patients) underwent primary PSARP, Group B (21 patients) underwent two-stage PSARP (PSARP with colostomy at the same stage followed by stoma closure 6 weeks later ). Group C (22 patients) underwent the traditional three- stage surgery (colostomy followed by definitive repair followed by colostomy closure). The children with associated syndromes and who presented with abdominal distension were assigned to group C. The patients with ARM were analyzed and categorized according to the type of malformation by the International Classification of Krickenbeck. All patients were subjected to meticulous clinical examination and routine laboratory investigations. Abdominal ultrasound was performed to exclude associated renal anomalies. Echocardiography was only requested for patients with suspected cardiac lesions.
PSARP was done under general anaesthesia, supplemented by a caudal block for postoperative analgesia. Oral feeding was started after regaining of the intestinal motility in all patients. An indwelling urinary catheter placed at operation and removed after approximately 3–4 days. Wound care was done by irrigation with ciprofloxacin and metronidazole solution and application of povidone iodine and metronidazole ointment. Patients were discharged when full oral feeding resumed with advice on colostomy care.
The patients were followed up in the outpatient clinic weekly for 1 month then every 3 months for 1 year, anal dilatation was started 2 weeks after the operation as per the Pena scheme [3]. In patients with colostomy, stoma closure was done after 6–8 weeks. During the follow up visits, the patients were examined to detect perineal excoriation, wound infection, wound dehiscence, anal stenosis or anal retraction, recurrence of fistula as well as complications of colostomy. The SPSS 16 software was used for data processing. Quantitative Data are expressed as mean (SD). Student’s t test and Oneway ANOVA with post-hoc Tukey HSD Test was used to compare the hospital stay and operative time. Qualitative data was expressed as proportions. Fisher’s exact test was applied for proportional comparisons of postoperative complications. P values of less than 0.05 were considered significant.
Results
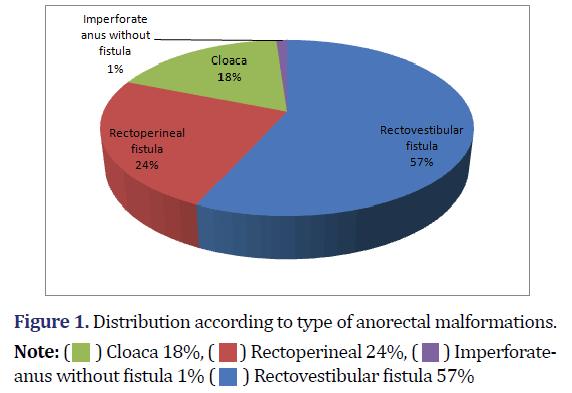
A total of 100 female patients presented with ARM. 10 patients were excluded from the study as 3 patients died after the first stage and 7 did not come for follow-up after first stage surgery. 16(17.8%) females who had persistent cloacal anomalies were excluded from the study. Therefore the study groups comprised a total of 74 patients. Only one patient with an imperforate anus without fistula presented with abdominal distension and was assigned to group C. Rest of the patients were randomly assigned to group A/B/C. There were 31 patients in Group A, 21 in Group B, and 22 in Group C. Pie diagram showing distribution according to type of Anorectal malformations (Figure 1).
The mean age of the three groups at the beginning of the study was the same; most of the patients were between 0-3 months of age. The age of patients at the time of surgery ranged from 1 day to 2 years. The average total length of hospital stay in Group A was 7.52 days, in Group B was 10.52 days and in Group C was 16.64 days. This difference was highly statistically significant.
The average total operative time in Group A was 116.45 minutes, in Group B was 237.00 minutes and in Group C was 256.19 minutes. The comparison of mean operative time among the three groups was found to be statistically significant (P=0.001). The mean operative time was highest in Group C and lowest in Group A. demographic data shown in Table 1. Twenty-six patients (35.4 %) in our study developed postoperative complications during the short-term follow up (Table 2).
| Groups | Post-hoc tukey | |||||
|---|---|---|---|---|---|---|
| A | B | C | A-B | A-C | B-C | |
| Age (months) | 3.33 ± 4.67 | 11.24 ± 7.32 | 13.25 ± 7.67 | 0.001* | 0.001* | 0.566, NS |
| Duration of hospital stay (days) | 7.52 ± 1.91 | 10.52 ± 2.84 | 16.64 ± 5.67 | 0.014* | 0.001* | 0.001* |
| Total operative time (minutes) | 116.45 ± 17.04 | 237.00 ± 21.55 | 256.19 ± 52.03 | 0.001* | 0.001* | 0.145, NS |
| Note: * Significant | ||||||
| Complications | Group | c2 value | P value | Fisher’s Exact P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group C | A-B | A-C | B-C | ||||
| (n=31) | (n=21) | (n=22) | |||||||
| Perineal excoriation | 19 | 5 | 2 | 17.035, df=2 | 0.001* | 0.011* | 0.001* | 0.240, NS | |
| 61.30% | 23.80% | 9.10% | |||||||
| Wound infection | 16 | 3 | 1 | 16.868, df=2 | 0.001* | 0.008* | 0.001* | 0.345, NS | |
| 51.60% | 14.30% | 4.50% | |||||||
| Wound dehiscence | 9 | 0 | 1 | 11.183, df=2 | 0.003* | 0.007* | 0.033* | 1.000, NS | |
| 29.10% | 0.00% | 4.50% | |||||||
| Anal stenosis | 2 | 0 | 0 | 2.851, df=2 | 0.240, NS | 0.509, NS | 0.505, NS | 1.000, NS | |
| 6.50% | 0.00% | 0.00% | |||||||
| Recurrence of fistula | 1 | 0 | 0 | 1.406, df=2 | 0.495, NS | 1.000, NS | 1.000, NS | 1.000, NS | |
| 3.20% | 0.00% | 0.00% | |||||||
| Anterior anal retraction | 0 | 0 | 0 | - | - | - | - | - | |
| 0.00% | 0.00% | 0.00% | |||||||
| Note: * Significant, NS- Non significant | |||||||||
In Group A, 16 (51.6%) patients had wound infections. Ten patients improved with antibiotics, whereas 6 (19.4%) patients progressed to wound dehiscence. Out of 6 patients with wound dehiscence, 5 patients underwent diverging colostomy to control the infection while one patient responded to conservative management. In Group B, 3 (14.3%) patients had wound infections, all responding to antibiotics. There was no (0 %) incidence of wound dehiscence in Group B (two-stage repair). In Group C, only 1 (4.5%) patient had wound infection and wound dehiscence. Anal stenosis in Group A was noticed in 2 (6.5%) patients, one required Y-V anoplasty and the other one required redo-PSARP due to associated anterior anal migration. However, in groups B and C, there was no occurrence of anal stenosis. There was no statistically significant association seen between anal stenosis and the groups (P=0.240). Recurrence of fistula was seen in 1 (3.2%) patient in Group A, secondary to wound dehiscence and none in Group B and Group C. The difference was not significant statistically.
Redo PSARP was required in 2 cases in Group A. One had recurrence of fistula to its original position inside the vestibule secondary to severe wound infection and fibrosis . The other patient has anal stenosis and anterior anal retraction. In group B and C, none of the patients required redo PSARP. There was no statistically significant association seen between revision PSARP and the groups (P=0.114). Peristomal skin excoriation was seen in 3 (14.3%) patients of Group B and 11 (50%) patients of Group C. All were treated with local application of zinc oxide and calamine ointment and all of them improved after colostomy closure. There were no other stomal complications in any of the groups.
Discussion
Posterior Sagittal Anorecto Plasty (PSARP), described by de Vries and Pena, is the preferred treatment for ARM today. Pena recommended performing a covering colostomy in cases of Anorectal malformation [3]. Some authors have preferred three stages rather than one stage procedure for the repair of female ARM. They stated that the occurrence of perineal wound complications would compromise the functional outcome. Therefore, colostomy has been advised to get the best results [5,6]. However, others argued that one stage repair of female ARM is feasible, safe and has a lot of advantages [7-9]. Selecting the single-stage or multi-stage repair of Anorectal malformation has been a topic of debate for years.
In our study, the most common type of ARM in females was found to be Recto Vestibular Fistula (RVF) in 56.6% of all female ARMs. The perineal fistula was the next common type, present in 24.4% of cases. Imperforate anus has the least incidence, present in only 1.1% of patients. These results were congruent with Stephens and Smith’s paper [10].
The incidence of loss to follow up after colostomy, in our study was 7%, the patients continued to live the colostomy without definitive repair. In developing countries, the increased cost of 3-stage operations has been highlighted in previous articles [10,11]. Our findings are in agreement with the findings of Adeniran [10] that a large number of patients, 50% in their experience, are lost to follow-up after a colostomy. Gangopadhyay et al. experienced that a lot of parents initially refuse treatment only by the thought of three surgeries over a span of 6–8 months [8]. Where possible, a two-stage surgery will reduce the total cost of treatment and hospital stay with obvious benefit both to the parents and the child, provided that the results are comparable with three-stage.
In this study, the rate of wound infection and wound dehiscence was significantly higher in group A (51.6% in Group A vs. 14.3% in group B and 4.5% in Group C, 19.4% in Group A vs. 0% in Group B vs. 4.5% in Group C respectively).The rates of wound infection and wound dehiscence were statistically comparable in Group B and Group C. The higher rate of wound complications in Group A (one-stage repair) is due to the absence of colostomy as a faecal diversion route and contamination of the wound by faecal matter. Louise Tofft, et al. in 2019 concluded that wound dehiscence occurred to a significantly lesser degree among patients with a colostomy [12,13].
In our study, although routine anal dilatation was done in all patients postoperatively to prevent anal stenosis, still anal stenosis occurred in 6.5% of patients in group A. There was no incidence of anal stenosis in Group B and Group C. Although not statistically significant, the higher rates of anal stenosis are mainly because the rate of wound complications was higher in Group A. Khalifa, et al. reported a significantly high incidence of anal stenosis in one stage (33.3%) when compared to two-stage PSARP (10.9%) [5].
In our study two patients required redo PSARP in Group A. There was no requirement of redo PSARP in Group B and Group C. Although this result is not statistically significant, similar results were reported in other studies. Elsaied et.al, reported that 40% of patients treated by one- stage procedure required redo PSARP while none of the patients treated by two-stage procedure needed a redo surgery and they considered the advantages of one stage in the correction of RVF is overrated [6]. Khalida Shreef, et al. reported that 20.8% in one stage group required redo ASARP while in the two-stage group only one patient (2.1%) required redo operation [5].
The complications of colostomy occurred in 16 patients (21.6 %). The most common complication of colostomy was peristomal skin excoriation, which was managed successfully with local treatment. The incidence of colostomy-related complications ranges from 28% to 74% in various studies [14]. However, all complications were mild and tolerable. The complications of colostomy cannot outweigh the protective effects of a stoma on preventing wound complications and the subsequent functional outcome. Therefore, a covering colostomy is still considered the safest way to avoid these complications.
Treatment of group B patients involved less operative time and they experienced a shorter hospital stay compared with group C and a statistical significance was found. The duration of hospital stay and total operative time was found to be lowest in Group A. However, if we consider the fact that the rate of wound complications is significantly higher in Group A, we feel that the advantages of one-stage operation are overrated. We also believe that the complications of colostomy are temporary and tolerable if we can achieve a sound operation and a continent child.
Conclusion
The following conclusions were drawn from this study
1. A diverging colostomy is vital in the management of Anorectal malformation to achieve a continent child. Without colostomy, wound complications may result in disruption of the entire repair and functional compromise.
2. Both two-stage and three-stage surgery have comparable outcomes in regard to the wound complications. Two- stage surgery has the additional advantage of omission of one stage, better compliance to treatment, and reduced cost of treatment. Therefore, two-stage PSARP can be encouraged as the standard management of female Anorectal malformation.
Limitations of the Study and Future Research
Further studies are required to compare the long-term complications and outcomes in terms of continence and constipation rate in one-stage, two-stage, and three-stage surgery.
References
- Levitt MA, Peña A. Anorectal malformations. Orphanet J Rare Dis 2007;2:33.
[Crossref] [Google Scholar] [Pubmed]
- Holschneider AM, Hutson JM. Anorectal malformations in children: Embryology, diagnosis, surgical treatment, follow-up. Berlin, Germany, Springer; 2016.
- De Vries PA, Peña A. Posterior sagittal anorectoplasty. J Pediatr Surg 1982;17(5):638–43.
[Crossref] [Google Scholar] [Pubmed]
- Gangopadhyay AN, Pandey V. Controversy of single versus staged management of anorectal malformations. Indian J Pediatr 2017;84(8):636–42.
[Crossref] [Google Scholar] [Pubmed]
- Shreef K, Khalifa M, Al Ekrashy M, Gobran T. One or two stages procedure for repair of rectovestibular fistula: Which is safer? (A single institution experience). Afr J Paediatr Surg 2017;14(2):27-31.
[Crossref] [Google Scholar] [Pubmed]
- Elsaied A, Aly K, Thabet W, Magdy A. Two-stage repair of low anorectal malformations in girls: is it truly a setback?. Ann Pediatr Surg 2013;9(2):69–73.
- Moore TC. Advantages of performing the sagittal anoplasty operation for imperforate anus at birth. J Pediatr Surg 1990;25(2):276–7.
[Crossref] [Google Scholar] [Pubmed]
- Gangopadhyaya AN, Kumar V, Upadhyaya VD, Chowdhary S, Srivastava A, Gupta DK, et al. Single-stage repair versus traditional repair of high anorectal malformations, functional results’ correlation with Kelly’s score and postoperative magnetic resonance imaging findings. Ann Pediatr Surg 2013;9(3):108-13.
- Menon P, Rao KLN. Primary anorectoplasty in females with common anorectal malformations without colostomy. J Pediatr Surg 2007;42(6):1103–6.
[Crossref] [Google Scholar] [Pubmed]
- Stephens FD, Smith ED. Classification, identification, and assessment of surgical treatment of anorectal anomalies. Pediatr Surg Int 1986;1(4) :200-5.
- Adeniran JO. One-stage correction of imperforate anus and rectovestibular fistula in girls: Preliminary results. J Pediatr Surg 2002;37(6):16–9.
[Crossref] [Google Scholar] [Pubmed]
- Liu G, Yuan J, Geng J, Wang C, Li T. The treatment of high and intermediate anorectal malformations: One stage or three procedures?. J Pediatr Surg 2004;39(10):1466–71.
[Crossref] [Google Scholar] [Pubmed]
- Tofft L, Salö M, Arnbjörnsson E, Stenström P. Wound dehiscence after posterior sagittal anorectoplasty in children with anorectal malformations. Biomed Res Int 2018;2018:2930783.
[Crossref] [Google Scholar] [Pubmed]
- Millar AJ, Lakhoo K, Rode H, Ferreira MW, Brown RA, Cywes S, et al. Bowel stomas in infants and children. A 5-year audit of 203 patients. S Afr J Surg 1993;31(3):110-3.
[Google Scholar] [Pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.








 ) Cloaca 18%, (
) Cloaca 18%, ( ) Rectoperineal 24%, (
) Rectoperineal 24%, ( ) Imperforateanus without fistula 1% (
) Imperforateanus without fistula 1% ( ) Rectovestibular fistula 57%
) Rectovestibular fistula 57%