Research Article - Archives of Clinical and Experimental Surgery (2025)
Colonic atresia and Hirschsprung’s disease Concurrence-A Myth or A Reality
Maneesh Kumar Joleya*, Ashok Laddha, Vinod Raj, Pooja Tiwari, Shashi Shankar Sharma, Ram Mohan Shukla, Brijesh Lahoti and Manoj JoshiManeesh Kumar Joleya, Department of Department of Pediatric Surgery, SSH and MGMMC, Indore, India, Email: drjollymaneesh@yahoo.co.in
Received: 27-Jan-2025, Manuscript No. EJMACES-25-165264; Editor assigned: 30-Jan-2025, Pre QC No. EJMACES-25-165264 (PQ); Reviewed: 13-Feb-2025, QC No. EJMACES-25-165264; Revised: 21-Apr-2025, Manuscript No. EJMACES-25-165264 (R; Published: 19-May-2025
Abstract
Background/Purpose: Colonic Atresia (CA) is a rare cause of bowel obstruction in neonates. The present study was designed to discuss surgical management of this rare entity with special emphasis on its association with Hirschsprung’s Disease (HD) which is often missed.
Methods: All cases of CA who presented to our centre from 1st January 2017 to 31st December 2021 were retrospectively reviewed and data was collected regarding type of atresia, surgical management done, outcome, whether histopathology was done and association with HD.
Results: The study reviewed 7 new-borns with CA treated in our centre (5 cases of type III, 2 cases of type II) with 1 having associated Anorectal Malformation (ARM). All the cases were diagnosed based on intraoperative finding and initial surgical management was done by performing a proximal stoma and distal mucous fistula and sending a biopsy above the peritoneal reflection to rule out HD. One case had anastomotic leak after stoma closure and diagnosed with HD on colonic biopsy after the leak. Two out of seven patients (28.6%) had associated HD which is quiet a big number to emphasis on making colostomy and taking biopsy as primary surgery rather than doing primary anastomosis in cases of CA.
Conclusions: Due to the rarity of colonic atresia its diagnosis and management may be challenging. Association of HD with CA is usually picked up after failure of primary anastomosis leading to high morbidity and mortality. Thus, staged surgery by making a diversion colostomy primarily and then definitive procedure after ruling out Hirschsprung’s disease should be the preferred option in centers without facilities of frozen section biopsy.
Keywords
Colonic atresia; Hirschsprung’s disease; Gastro-intestinal atresia’s; Aganglionosis; Large bowel obstruction; Large bowel atresia
Introduction
Primary Colonic atresia (CA) is an infrequent cause of neonatal intestinal obstruction [1]. Among all gastrointestinal atretic conditions, CA constitutes between 2% and 15% of documented cases [2,3]. Epidemiological studies demonstrate considerable variation in CA occurrence, with reported frequencies ranging between 1:1500 [4] and 1:66,000 live births [5]. This marked rarity poses significant diagnostic and therapeutic challenges for pediatric surgeons. CA is associated with various abdominal anomalies (abdominal wall defects, malrotation, multiple intestinal atresia and HD Hirschsprung’s disease) and extra abdominal anomalies (musculoskeletal, ocular, and facial anomalies) [6]. Association of CA with HD creates a dilemma in surgical decision making as it is often missed in emergency. HD is recognized in at least 2%-8.4% of patients with colonic atresia [7-11]. Some authors have hypothesized that when a vascular insult occurs before retroperitoneal fixation of the colon at 11 weeks’ gestation, caudal migration of the myenteric neurons is interrupted [12]. Therefore it is imperative to rule out Hirschsprung disease with suction rectal biopsy or full thickness or seromuscular rectal biopsy or frozen section biopsy, before reestablishing intestinal continuity in every patient with colonic atresia.
Case Presentation
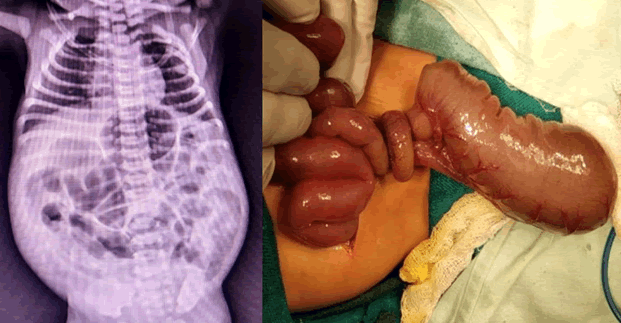
We conducted a comprehensive retrospective analysis of seven CA cases treated at our institution during a five-year period (January 2017 through December 2021). The clinical data gestational age, gender, age at presentation, presenting symptom, associated anomalies, diagnostic tools, site and variety of atresia, type of surgical intervention histopathology report and outcome were recorded and analyzed. Grosfield’s classification was used to determine the type of atresia [13] (Figures 1 and 2).
Results
The study reviewed 7 new-born with CA treated in our centre (5 cases of type III, 2 cases of type II) with 1 having associated ARM. The main presenting features were not passing motion since birth, gradually progressive abdominal distension and vomiting. Initial surgical treatment of CA was fashioning stoma proximally and mucous fistula distally with biopsy of distal segment in all our patients. Details of the cases was recorded in tabular form (Table 1).
| S.no | GA | Age/Gender | Type of presentation | Diagnostic tool Intra-operative finding | Type of atresia | Surgical procedure | Biopsy (Hirschsprung's disease) |
Outcome |
|---|---|---|---|---|---|---|---|---|
| 1. | FT | PND 3/F | Not passing meconium since birth with absent anal opening Abdominal distension for 2 days |
1) Dilated proximal and mid transverse colon with atresia at junction of mid and distal transverse colon 2) Associated necrotizing enterocolitis 20 cm proximal to IC junction about 10 cm of ileum was involved |
IIIa | 1) Exploratory laparotomy with resection and anastomosis of ileum with transverse colostomy and distal mucus fistula and distal rectal biopsy 2) PSARP after 6 weeks 3) Stoma closure which leaked after 6 weeks 4) Stoma again refashioned 5) Stoma closure done |
No HD | Alive |
| 2. | FT | PND 3 F |
Not passing motions since birth gradually progressive abdominal distension and bilious vomiting |
Atresia at distal transverse colon | IIIa | 1) Exploratory laparotomy with end colostomy and mucus fistula with biopsy | No HD | Alive |
| 3. | FT | 4 days M |
Gross distension of abdomen Non-passage of stools Bilious vomiting |
Atresia at distal transverse colon | II | 1) Exp. lap with transverse Colon stoma with distal rectal biopsy and sigmoid as mucus fistula 2) Stoma closure at 1 year (Passed motion after 13 days) |
No HD | Alive |
| 4. | FT | 2 days F |
Features of acute intestinal obstruction | Distal transverse colon atresia | II | 1) Exp. lap with transverse colon as proximal stoma and sigmoid (microcolon) as mucus fistula 2) Colostomy closure done at 6 months of age but anastomosis leaked 3) Santulli Chimney stoma was made and excised distal colon sent for HPE 4) Duhamel pull through |
Hirschsprung's disease was associated | Alive |
| 5. | FT | 5 D/M | Huge distension of abdomen Non-passage of stools |
Atresia at proximal transverse colon | IIIa | 1) Exploratory laparotomy with proximal transverse colostomy and distal transverse colon mucus fistula with distal rectal biopsy | No HD | Died |
| 6. | FT | 4D/M | Distension of abdomen Non-passage of stools Bilious vomiting |
Atresia at distal transverse colon | IIIa | 1) Exploratory laparotomy with proximal colostomy (transverse colon) and distal mucus fistula with rectal biopsy 2) Soaves procedure was done |
Hirschsprung's disease was associated | Alive |
| 7. | FT | 3D/M | Distension of abdomen Non-passage of stools |
IIIa | 1) Exploratory laparotomy with end colostomy and mucus fistula | No HD | Alive | |
| 8. | FT | 3D /M | Not passing motion since birth |
Table 1. Patient’s characteristics, surgical management and outcome.
Case 1: A 3-day-old female neonate (birth weight: 2.5 kg) presented with complete absence of meconium passage since birth and gross abdominal distension for 2 days. Diagnosed as a case of ARM with intestinal obstruction and planned for exploratory laparotomy as we suspected ileal atresia with ARM. Intra-operatively there was dilated proximal and mid transverse colon with atresia at junction of mid and distal transverse colon type IIIa atresia with associated necrotizing enterocolitis of ileal segment 20 cm proximal to IC junction patient underwent resection and anastomosis of ileum with transverse colostomy and distal mucus fistula with biopsy of distal rectal segment. Postoperative period was uneventful. Posterior Sagittal Ano-Rectoplasty (PSARP) was done after 6 weeks as distal segment histopathology report was not suggestive of HD. Stoma closure was planned after six weeks when appropriate size dilator was negotiated from below. Unfortunately, anastomosis leaked for which stoma again refashioned. Later on stoma closure was done and patient is doing well on follow up.
Case 2: Post-natal day 3 female child weighing 2.5 kg presented with complains of not passing motion and gross abdominal distension and bilious vomiting since birth. Patient underwent exploratory laparotomy and intra-operatively CA was found at distal transverse colon (type IIIa atresia) for which end colostomy and mucus fistula with biopsy from peritoneal reflection was done. Histopathology report was not suggestive of HD.
Case 3: Four days old male child admitted with complains of gross distension of abdomen, nonpassage of stools andbilious vomiting since birth. On exploration distal transverse colonic atresia was found (type II atresia) initially managed by transverse colon stoma with full thickness distal rectal biopsy and sigmoid colon as mucus fistula. Histopathology report did not show any features of HD. But patient turned up late so stoma closure was done at age of 1 year.
Case 4: Two days old female child admitted with features of acute intestinal obstruction. On exploration it was found to bedistal transverse colonic atresia was found (type II atresia) initially managed with transverse colon as proximal stoma and sigmoid colon (microcolon) as mucus fistula. Later on, colostomy closure was done at 6 months of age but anastomosis leaked so Santulli Chimney stoma was made and excised distal colon sent for HPE which was suggestive of HD. As definitive procedure Duhamel pull through was done. Presently patient is doing well.
Case 5: A 5-day-old full-term male child admitted for huge distension of abdomen and non-passage of stools since birth was diagnosed as intestinal obstruction planned for exploratory laparotomy. Intra-operative finding was atresia at proximal transverse colon suggestive of type IIIa atresia for which proximal transverse colostomy and distal transverse colon mucus fistula with distal rectal biopsy. Histopathology report was not suggestive of HD.
Case 6: Day 4 full term male child admitted with complains of gross distension of abdomen, nonpassage of stools and bilious vomiting. On exploration there was atresia at distal transverse colon consistent with type IIIa atresia. It was managed with proximal colostomy (transverse colon) and distal mucus fistula with rectal biopsy. Histopathology report was suggestive of HD for which Soave’s procedure was done and patient is doing well at present.
Case 7: A 3-day-old full-term male child admitted for gross distension of abdomen and non-passage of stools since birth diagnosed as intestinal obstruction planned for exploratory laparotomy. Intra-operative finding was suggestive of type IIIa atresia which was managed with end colostomy and distal mucus fistula with rectal biopsy. Histopathology report did not show any features of HD.
Discussion
Contemporary understanding of CA etiology emerged from Louw and Barnard’s groundbreaking research, which identified mesenteric vascular compromise during fetal development as the primary pathogenic mechanism. Haematological events in vivo such as embolus from the placenta or spontaneous thrombosisor mechanical events (volvulus, intussusception or strangulated internal herniation) can cause segmental ischemia [8].
CA has been found to be associated with vesicointestinal fistula, Hirschsprung’s disease, omphalocele, gastroschisis, exomphalos, choledochal cyst and imperforate anus [9]. Rarely CA is associated with extra abdominal anomalies likefacial anomalies, congenital heart disease, hypoplasia of abdominal aorta, ophthalmic, renal, brain defects, encephalocele, and musculoskeletal anomalies. The presence of associated major anomalies with CA has a poor prognosis [10]. In our study the major associated anomalies were HD (which led to anastomotic leak in one of our cases) anorectal malformation and necrotizing enterocolitis.
CA presents from birth with typical features of obstruction likedistention of abdomen, bilious vomiting and non-passage of meconium. Plain X-rays typically show dilatation of proximal bowel loops. The diagnosis is usually confirmed by contrast enema studies showing a narrowed distal colon with sudden cessation of contrast at the level of the atresia. Contrast studies were not done in our patients as all of them presented late with huge distension and bilious vomiting and were explored on the same day. Classification of intestinal atresia applied to CA was given by Grosfeld. According to this classification, type I defect represents a defect in mucosa with an intact mesentery; type II defect consists of atretic bowel ends connected by fibrous band ; type IIIa defect consists of V-shaped mesenteric gap defect between the atretic segment, whereas type IIIb lesion consists of the apple-peel deformity, where there is proximal colonic atresia and the distal bowel is supplied by a single retrograde blood vessel; type IV lesion describes instances of multiple atresia (“string of sausage” effect). Most cases presented with type IIIa defects [7] as were seen in our series as well.
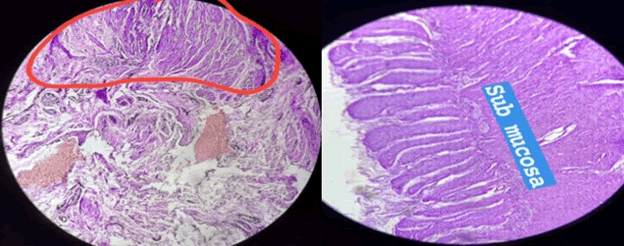
Our surgical approach differentiated based on anatomical location: lesions proximal to the splenic flexure underwent primary resection and anastomosis after frozen section biopsy, and for atresia distal to splenic flexure colostomy with delayed anastomosis [11-13]. Two (28.6%) of our patients had associated HD. In one of them (as distal biopsy was not sent during initial surgery) the bowel anastomosis leaked on third postoperative day and santualli like procedure was done with biopsy sent from distal segment sent to rule out HD. In the post-operative period patient was losing significant amount of stomal effluent as distal segment was aganglionic. The biopsy from distal bowel showed absence of ganglionic cells and hypertrophied nerve fibres. Later on, as definitive treatment modified Duhamel procedure was done and patient had an excellent outcome we learnt a lesson from this incident. Also, there is technical issue in primary anastomosis due to discrepancy between the luminal sizes of the distal and proximal bowels in CA patients [14,15]. As per our experience proximal diversion colostomy with biopsy from rectum and distal mucous fistula should be done followed by definitive procedure (Biopsy is must to rule out H.D.) like in our setup where frozen section facility is not available.
Incidence of coexistence of CA and HD ranges from 2 to 8.4 % which is difficult to diagnose and treat [16]. The exact aetiological association between CA–HD is unknown. Some hypotheses suggests that during 5–12 weeks of gestation cranio-caudal migration of neural crest cells into the bowel explains association of CA and aganglionosis. During antenatal period bowel proximal to transitional zone with pre-existing HD causes dilatation and meconium impaction resulting in intrauterine segmental volvulus with mesenteric vascular insufficiency and secondary CA at the same segment. Common genetic origin of CA and HD explains the coexistence of two congenital disorders [17-20].
Failure of anastomosis following restoration of intestinal continuity is usually considered as diagnostic of coincident HD. In order to avoid functional intestinal obstruction or anastomotic dehiscence biopsies of the distal colon or rectum should be performed either during the initial laparotomy or before re-establishing intestinal continuity to reduce morbidity and mortality. In centres with frozensection biopsy facilities, decision can be made on the operation table itself. The mortality rate of CA is 10% and majority of reports in published literature show it due to anastomotic leak after primary resection and anastomosis in case of CA.
Conclusion
This case series highlights crucial considerations for managing CA in resource-limited settings where intraoperative frozen section analysis is unavailable biopsy of proximal stoma, distal mucous fistula and rectum should be done. We also reiterate the fact that rectal biopsy must be performed to exclude HD before establishing intestinal continuity in any case of colonic atresia to reduce the mortality rate associated with missed diagnosis of HD.
Consent for Publication
Written consent was obtained.
Availability of Data and Material
Data is available with the authors on request.
Competing Interests
No potential conflict of interest relevant to this article was reported.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Authors Contributions
Conceptualization: M.J. Data curation: S.S.S. Formal analysis: P.T., V.R. Supervision: B.K.L. Validation: M.J.O. Writing-original draft: M.J. Writing-review and editing: M.J., R.M.S.
Acknowledgements
We would like to acknowledge Pediatric Surgery team at Superspeciality & M.Y. Hospitals, for their support to this work, and their ongoing and continuous efforts with CA individuals and their families.
References
- Dalla Vecchia LK, Grosfeld JL, West KW, Rescorla FJ, Scherer LR, Engum SA. Intestinal atresia and stenosis: A 25-year experience with 277 cases. Arch Surg 1998;133(5):490-497.
[Crossref] [Google Scholar] [PubMed]
- Freeman NV. Congenital atresia and stenosis of the colon. British J Surg 1966;53(7):595-599.
- Powell RW, Raffensperger JG. Congenital colonic atresia. J Pediat Surg 1982;17(2):166-170.
[Crossref] [Google Scholar] [PubMed]
- Sturim HS, Ternberg JL. Congenital atresia of the colon. Surgery 1966;59(3):458-464.
[Google Scholar] [PubMed]
- Davenport M, Bianchi A, Doig CM, Gough DC. Colonic atresia: Current results of treatment. J Royal Coll Surg Edinbur 1990;35(1):25-28.
[Google Scholar] [PubMed]
- Etensel B, Temir G, Karkiner A, Melek M, Edirne Y, Karaca I, et al. Atresia of the colon. J pedia Surg 2005;40(8):1258-1268.
[Crossref] [Google Scholar] [PubMed]
- Park J. Delayed diagnosis of Hirschsprung's disease associated with colonic atresia and multiple anomalies: Report of a case and review of the literature. J Pedia Surg Case Rep 2016;10:20-22.
- Grosfeld JL, Ballantine TV, Shoemaker R. Operative management of intestinal atresia and stenosis based on pathologic findings. J Ped Surg 1979;14(3):368-375.
[Crossref] [Google Scholar] [PubMed]
- Erskine JM. Colonic stenosis in the newborn: The possible thromboembolic etiology of intestinal stenosis and atresia. J Pedia Surg 1970;5(3):321-333.
[Crossref] [Google Scholar] [PubMed]
- Soni V, Valse PD, Vyas S. Colonic atresia due to internal herniation through the falciform ligament defect: A case report. J Neonatal Surg 2014;3(2):21.
[Google Scholar] [PubMed]
- Komuro H, Takahashi MI, Matoba K, Hori T, Hirai M, Gotoh C, et al. Rare association of severe hypoplasia of the abdominal aorta with imperforate anus, colonic atresia and choledochal cyst. Pedia Surg Int 2006;22:289-292.
[Crossref] [Google Scholar] [PubMed]
- Benson CD, Lotfi MW, Brough AJ. Congenital atresia and stenosis of the colon. J Pedia Surg 1968;3(2):253-257.
[Crossref] [Google Scholar] [PubMed]
- DeFore Jr WW, Garcia-Rinaldi R, Mattox KL, Harberg FJ. Surgical management of colon atresia. Surg Gynecol Obstet 1976;143(5):767-769.
[Google Scholar] [PubMed]
- Watts A, Sabharwal A, MacKinlay G, Munro F. Congenital colonic atresia: Should primary anastomosis always be the goal? Pediac Surg Int 2003;19:14-17.
[Crossref] [Google Scholar] [PubMed]
- Oldham KT, Arca MJ. Atresia, stenosis and other obstructions of the colon. Pedia Surg 1998:2080-2082.
- Akgür FM, Tanyel FC, Büyükpamukçu N, Hiçsönmez A. Colonic atresia and Hirschsprung's disease association shows further evidence for migration of enteric neurons. J Pedia Surg 1993;28(4):635-636.
[Crossref] [Google Scholar] [PubMed]
- Croaker GD, Harvey JG, Cass DT. Hirschsprung's disease, colonic atresia and absent hand: A new triad. J pedia Surg 1997;32(9):1368-1370.
[Crossref] [Google Scholar] [PubMed]
- Akgur FM, Olguner MU, Hakguder G, Ozer E, Aktug T. Colonic atresia associated with Hirschsprung's disease: It is not a diagnostic challenge. European J Pedia Surg 1998;8(6):378-379.
[Crossref] [Google Scholar] [PubMed]
- El-Asmar KM, Abdel-Latif M, El-Kassaby AH, Soliman MH, El-Behery MM. Colonic atresia: Association with other anomalies. J Neon Surg 2016;5(4):47.
[Crossref] [Google Scholar] [PubMed]
- J Park. Delayed diagnosis of Hirschsprung’s disease associated with colonic atresia and multiple anomalies: Report of a case and review of the literature. J Ped Surg Case Rep 10(2016):20-22.