Research Article - Archives of Clinical and Experimental Surgery (2025)
Does Transinguinal Preperitoneal Repair (Tipp) has an Edge Over Lichtensteinâs Repair? A Comparative Study
Guru Prasad, Jahid Husain S*, Pratheep Karthick P, Moparthy Venkatesh and Gowtham KJahid Husain S, Department of General Surgery, ACS Medical College, Chennai, India, Tel: +919940340953, Email: husainj27@gmail.com
Received: 06-Jan-2025, Manuscript No. EJMACES-25-157903; Editor assigned: 08-Jan-2025, Pre QC No. EJMACES-25-157903; Reviewed: 23-Jan-2025, QC No. EJMACES-25-157903; Revised: 30-Jan-2025, Manuscript No. EJMACES-25-157903; Published: 06-Dec-2024
Abstract
Background: Many procedures had been advocated for inguinal hernia repair. Herniorraphy had been overshadowed by Lichtenstein’s mesh repair but off late it has been advocated placing a preperitoneal mesh has less complications. The aim of this study is to compare Transinguinal Preperitoneal Repair (TIPP) with Lichtenstein repair. Materials and methods: This was a prospective comparative study of adult age>18 years who had undergone inguinal hernia repair over one-year period between June 2023 to May 2024 with a minimum follow up period of 6 months. The age, presenting symptoms, side of the hernia, interval between symptom and presentation, operative procedure performed, intra-operative finding/content of the hernia sac, post-operative complications, duration of hospital stay, outcome of treatment and recurrence rates were assessed. Results: A total of 100 cases of inguinal hernia repairs were undertaken. Out of this number, 50 underwent Lichtenstein repair and 50 underwent transinguinal preperitoneal repair. There was no difference in acute pain in both the arms. Seroma was the second most common post-operative complication which was statistically significant in the Lichtenstein repair arm. While chronic inguinodynia was found more in Lichtenstein repair and in the same arm four recurrences occurred, two within 6 months and the other two after a year. Conclusion: Inguinal hernia repair is a constantly evolving entity. TIPP repair has few acute complications and seem to have lesser chronic complications compared to Lichtenstein repair. Maybe the time has arrived for a paradigm shift in treating inguinal hernias.
Keywords
Inguinal hernias; Hernioplasty; Hernial contents; Lichtenstein; Preperitoneal
Introduction
Groin hernias are a common entity in surgical practice with much higher percentage occurring in men than women. Approximately 75% of abdominal wall hernias occur in the groin. The lifetime prevalence of groin hernias is 27% in men and 3% in women. The frequency of groin hernia repair rises from 0.25% in patients 18 years of age to 4.2% in patients 75 to 80 years of age [1]. Patients with a groin hernia may report a bulge in the groin that becomes progressively larger over time. Most patients with groin hernias report pain or vague discomfort, but up to one-third of patients have no symptoms [2]. Symptoms may worsen with standing, straining, lifting, or coughing. Patients may report having symptoms only at the end of the day or after prolonged activity and that the bulge disappears when they are lying flat. However, the absence of a reducible mass or palpable defect does not rule out a hernia.
After much deliberation in the methods of repair Herniorraphy where we strengthen the weakened Inguinal region by using normal anatomical structures present in the vicinity was advocated. Various herniorraphy techniques were advocated by individual surgeons claiming superiority of one over the other and the debate lasted close to a century with still recurrences occurring at a significant rate. Then Lichtenstein came up with the idea of a mesh between the anatomical structures without having to pull these structures to bring them together. The mesh would cause fibrosis and still recurrences though not eliminated became low in comparison to Herniorraphy. For the last 4 decades Lichtenstein’s open hernia repair has been the standard of care for uncomplicated Inguinal hernias. Recently better understanding of the predisposing factors of hernia, the science behind occurrence of hernia suggested the most anatomical and best way of treating a hernia would be to reduce it and place a mesh in the preperitoneal layer.
Materials and Methods
We collected the data of all Inguinal hernia patients who reported to our hospital over the past one years from June 2023 to May 2024 prospectively, randomised them into either TIPP arm or the Lichtenstein repair arm and analysed the data. Ethical committee clearance was taken in this regard.
Inclusion criteria
Patients attending surgical OPD who are:
1. 18 years or more
2. Only Inguinal hernia patients
3. Willing to randomise into either arm
Exclusion criteria
1. Below 18 years
2. Femoral hernias and incisional hernias
3. Previously treated at another centre.
4. Recurrent hernias
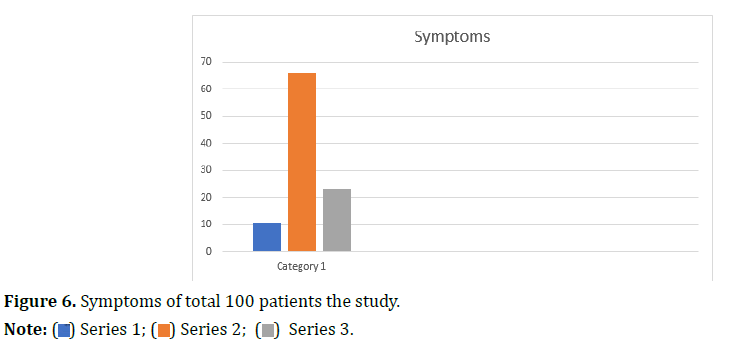
Standard examination was carried out by an expert surgeon. During the entire period patients were properly evaluated and recorded by photography systematically for comparison in future. In total there were 100 patients who were identified as having Inguinal hernias. They had undergone thorough clinical examination, imaging and other work up wherever necessary. The patients were subjected to surgery as an elective procedure either by TIPP method or Lichtenstein method as per the arm. At inguinal exploration, hernial sac was identified; hernial sac was opened first to look for the contents. During surgical exploration we avoided manual reduction of hernia content before opening the hernial sac. Once contents were identified, contents were reduced manually and hernial sac was dissected up to the deep ring. it was then transfixed, ligated and divided at deep ring and rest of the sac was removed. After dealing with the hernia intraoperatively by reducing the contents the posterior wall of the Inguinal canal was strengthened by in either of the two ways; hernioplasty by using a polypropylene mesh in the preperitoneal layer in the 50 patients of TIPP arm (Figures 1 and 2), and in the standard method Lichenstein repair where the mesh is placed anteriorly fixing it to conjoint tendon and Inguinal ligament in 50 patients (Figures 3 and 4). All the patients were followed up regularly for a minimum of 6 months post intervention to record and address any complications. Statistical analysis was performed using SPSS, version 18.0 software.
Results
Total Patients: 100
Transinguinal Preperitoneal arm: 50
Lichentstein repair arm: 50
Gender distribution
Male: 93
Female- 7
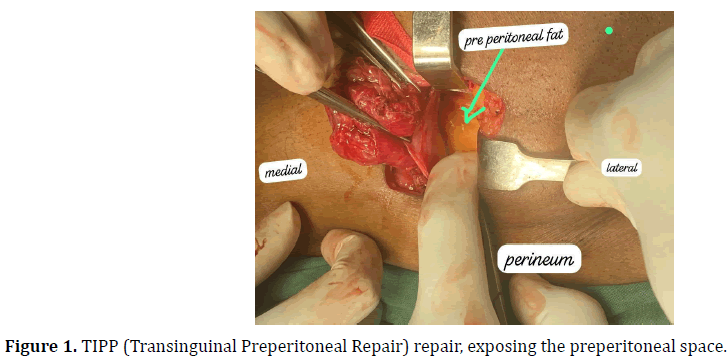
Age distribution
Age distribution of patients shown in Figure 5.
18 to 40: 26
40 to 60: 47
>60 yrs: 27
Median age of the patients 41 years
Mean interval between symptom and presentation: 6 months (3 to 14 months)
The mean duration of hospital stay: 1.3 days (1-3) in both the arms.
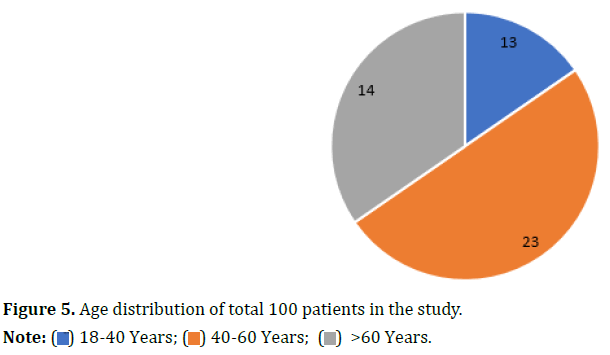
Symptoms
Symptoms of patients shown in Figure 6.
Groin pain without swelling: 11
Groin Swelling: 66
Groin swelling with pain: 23
Type of repair
Average intraoperative time;
TIPP–55 min
Lichtenstein repair–42 min
Hernial content and postop complications are shown in Tables 1 and 2.
| Content | Number | Percentage |
|---|---|---|
| Omentum | 52 | 52% |
| Small bowel | 26 | 26% |
| Large bowel | 16 | 16% |
| Ovary | 4 | 4% |
| Appendix | 2 | 2% |
| Total | 100 | 100% |
| Parameter | TIPP arm | Lichtenstein arm | p value |
|---|---|---|---|
| Acute pain | 16 | 18 | >0.05 (insignificant) |
| Scrotal edema | 4 | 8 | >0.05 (insignificant) |
| Seroma | 2 | 11 | <0.05 (significant) |
| Wound infection | 1 | 5 | >0.05 (insignificant) |
| Chronic inguinodynia | 2 | 16 | <0.05 (significant) |
| Recurrence | 0 | 3 | <0.05 (significant) |
Discussion
For the last four decades Lichtenstein’s open hernia repair has been the standard of care for uncomplicated Inguinal hernias. Recently better understanding of the predisposing factors of hernia, the science behind occurrence of hernia suggested the most anatomical and best way of treating a hernia would be to reduce it and place a mesh in the preperitoneal layer [3]. The laparoscopic methods of Total Extraperitoneal Repair (TEP) and Trans Abdominal Preperitoneal Repair (TAPP) came as to address the need of keeping a preperitoneal mesh and found success. But the problem is both these procedures have a steep learning curve, the anatomy is unconventional due to the inverse view, potential complication of large hematoma due to larger area of dissection and sometimes injuring blood vessels which are under vision and have better control in open surgery, also they come at multiple times the cost of open surgery. Lately the same endpoint can be achieved in the open method too [4,5].
In TIPP through Inguinal incision Inguinal canal opened, sac dissected, contents reduced and the transversal fascia carefully dissected and incised in the middle. Now a custom fit prolene mesh is placed in the preperitoneal layer. Though the abdominal pressure itself will retain the mesh in its place we sutured the mesh to conjoint tendon medially, internal oblique muscle superiorly and laterally. Then we closed the rent in transversalis fascia with absorbable suture. We did not approximate any other structures. We closed the incised external oblique fascia and skin. In the other arm standard Lichtenstein repair was done where the mesh is kept in the anterior layer above the internal oblique muscle with mooring stitches to pubic tubercle, Inguinal ligament, conjoint tendon and internal oblique muscle.
The outcomes of both the arms were analysed. The TIPP arm in the short term outcomes had less chances of seroma occurrence, wound infections, and is more physiological and long term complications like chronic inguinodynia, and recurrence in the six months’ time we followed up was high in TIPP arm which is similar to National and international studies [6,7]. More importantly we did not encounter any bleeding of concern or peritoneal breach during dissection in all the 50 cases, and is definitely equivalent if not superior to TEP and TAPP for the same result. TIPP needed 10 to 12 minutes extra operating time with respect to conventional Lichtenstein [8,9]. Since these were the initial days of the operating team even this time gap can be bridged soon. Also, an incision averaging 4 cm hidden in the groin is always welcome than scars at visible areas to some [10].
We expect that the mesh placement is easier comparatively than in males. In contrary the presence of spermatic cord in males serves as a guide to the surgeon while in female inguinal hernia the absence of cord makes the surgeon tread an unfamiliar territory.
That’s the reason surgeons might end up injuring the structures in the sac in females. If it is an injury to the bowel and we haven’t realised it might have dire consequences.
Conclusion
TIPP is an alternative method of tension free repair of Inguinal hernias with better results and validation by multicentric trials including more patients and replication of our results will establish its place in Inguinal hernia surgery. Maybe the time has arrived for a paradigm shift in treating inguinal hernias.
References
- Bax T, Sheppard BC, Crass RA. Surgical options in the management of groin hernias. Am Fam Physician 1999;59(4): 893-906.
[Google Scholar] [Pubmed]
- Townsend CM, Beauchamp RD, Evers BM. Sabiston textbook of surgery: The biological basis of modern surgical practice. 20th ed. Elsevier, 2017.
- Sajid MS, Craciunas L, Singh KK, Sains P, Baig MK. Open transinguinal preperitoneal mesh repair of inguinal hernia: A targeted systematic review and meta-analysis of published randomized controlled trials. Gastroenterol Rep (Oxf) 2013;1(2):127-137.
[Crossref] [Google Scholar] [Pubmed]
- Maiti S, Kushwaha P, Maiti KB. Modified lichtenstein technique for Transinguinal Preperitoneal Prosthesis (tipp) repair of groin hernia. Indian J Surg 2019;81:96-100.
- Khan HM. A comparative study of lichtenstein tension free mesh repair vs transinguinal pre-peritoneal mesh repair for inguinal hernias. J Cardiovascular Dis Res 2021; 12(4):1-5.
- Koning GG, Koole D, de Jongh MA, de Schipper JP, Verhofstad MH, Oostvogel HJ, et al. The transinguinal preperitoneal hernia correction vs Lichtenstein’s technique; is TIPP top?. Hernia 2011;15:19-22.
[Crossref] [Google Scholar] [Pubmed]
- Ray R, Kar M, Mukhopadhyay M. Transinguinal preperitoneal technique of inguinal hernioplasty–a better alternative to lichtenstein procedure. J Clin Diagn Res 2014;8(5):NC01.
[Crossref] [Google Scholar] [Pubmed]
- Bökkerink WJ, Koning GG, Malagic D, Hout LV, Laarhoven CJ, Vriens PW. Long-term results from a randomized comparison of open transinguinal preperitoneal hernia repair and the Lichtenstein method (TULIP trial). Br J Surg 2019;106(7):856-861.
[Crossref] [Google Scholar] [Pubmed]
- Patil SM, Dharmapuri A. A randomized controlled study of transinguinal pre peritoneal repair vs Lichtenstein repair for inguinal hernia. Int J Surg 2019;6(8):2757-2760.
- Silveira CA, Poli de Figueiredo SM, Dias YJ, Martin RR, Rasador AC, Fernandez MG, et al. Transinguinal Preperitoneal (TIPP) versus Lichtenstein for inguinal hernia repair: A systematic review and meta-analysis. Hernia 2023;27(6):1375-1385.
[Crossref] [Google Scholar] [Pubmed]











 ) 18-40 Years; (
) 18-40 Years; ( ) 40-60 Years; (
) 40-60 Years; ( ) >60 Years.
) >60 Years.