Research Article - Archives of Clinical and Experimental Surgery (2023)
Efficacy of Modified POSSUM Scoring System in Predicting Morbidity and Mortality in Cases of Perforated Peritonitis
Jahid Husain S1*, Gulam Nabi2, Milind H Iddalagi1 and Syed Saad32Department of General Surgery, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore, India
3Department of General Surgery, St. John’s Medical college, India
Jahid Husain S, Department of General Surgery, MVJ Medical College and Research Hospital, Bangalore, India, Email: husainj27@gmail.com
Received: 25-Aug-2023, Manuscript No. EJMACES-23-111212; Editor assigned: 28-Aug-2023, Pre QC No. EJMACES-23-111212 (PQ); Reviewed: 11-Sep-2023, QC No. EJMACES-23-111212; Revised: 18-Sep-2023, Manuscript No. EJMACES-23-111212 (R); Published: 25-Sep-2023
Abstract
Background: Even though surgical peritonitis being one of the most common problem faced by surgeons in emergency, still the post-operative period of perforated peritonitis is unpredictable most of the times and it carries considerable morbidity and mortality. It therefore becomes necessary for a scoring system that predicts the post-operative period.
There have been many scoring systems developed, including the American Society of Anesthesiologists (ASA) for general risk prediction, Acute Physiology and Chronic Health Evaluation III (APACHE III) for intensive care, and the Goldman Index for cardiac-related problems after surgery. In our study, we propose to use the modified POSSUM scoring to predicting the morbidity and mortality in perforated peritonitis.
Methods: Patients presenting to MVJ Medical College and Research Hospital, Hoskote from December 2020- November 2022 (24 Months). All cases of established peritonitis admitted in Department of General Surgery of MVJMC&RH. A total of 50 patients admitted who underwent emergency laparotomy for perforated peritonitis at MVJ Medical College and Research Hospital. Patients presenting with peritonitis was evaluated with detailed history and clinical examination and pre-operative physiological variables was collected and intra-operative variables were assessed and the expected outcome was measured by using POSSUM equation. Patient was followed up for 4 week after the surgery. Outcome and complications were recorded. Statistical analysis done by expected and observed outcome (chi-square test).
Results: In our study, 50 patients were studied and male outnumbered females. The most common site of perforation in gastrointestinal tract was gastric perforation followed by duodenum, ileum and appendix. Crude mortality rate of 10%. Crude morbidity rate of 60% and most of the patients presented with multiple complications. Maximum number of patients presented late >24 hrs and almost 50% mortality in the group where patient presented late (>48 hrs). Physiological variables such as cardiovascular system, blood pressure, hemoglobin, blood urea, serum potassium and operative variables such as operative complexity, multiple procedure, presence of malignancy, mode of surgery were significant. Additional factor perforation to operation time was included in our study and found to be significant. Predicted risk of mortality and morbidity was calculated and compared with the observed mortality and morbidity. An Observed to Expected ratio (O: E) for mortality was 1.020 (there was no significant difference between the predicted and observed values) (p=0.980) and for morbidity was 1.005 (there was no significant difference between the predicted and observed values) (p=0.934). For mortality and morbidity, positive predictive value was 80% and 97%, negative predictive value was 95% and 93%, sensitivity was 80% and 97%, specificity was 95% and 93% respectively. POSSUM score as it’s better at predicts mortality and morbidity, but it’s over predict morbidity in lower risk groups.
Conclusion: POSSUM scoring system is better since it’s include both physiological and operative parameters and can be used as a significant tool for predicting outcomes in perforated peritonitis. Factors such as cardiovascular system, blood pressure, hemoglobin, blood urea, serum potassium, operative complexity, multiple procedure, presence of malignancy, mode of surgery were significant to predict post-operative outcomes independently. Depends on the scoring system, patients attender can be counselled pre-operatively and prior correction of risk factors can be done. Strict vigilance and prompt adjustment of the verified parameters can improve the patient's overall health and decrease morbidity and mortality. Widespread awareness and education about perforated peritonitis, early referrals, early diagnosis and prompt treatment must be implemented to shorten the duration of perforation to operation time.
Keywords
Perforated peritonitis; POSSUM score; Surgery; POSSUM
Introduction
Surgical peritonitis remains one of the most common problems faced by surgeon”. It still remains as a major cause of morbidity and mortality (mortality from 10%-40%) [1]. The surgeons treating it know the dreadful and fatal complication; the problems can be minor wound infection to Systemic Inflammatory Response Syndrome (SIRS) or septic shock. Even if patients reach the hospital at the earliest, still the post-operative period is unpredictable most of the times [2]. It therefore becomes necessary for a scoring system that predicts the post-operative period. In our study, we propose to use the Modified POSSUM Scoring (Physiological and Operative Scoring System in Enumeration of Morbidity and Mortality) to predicting the morbidity and mortality in perforated peritonitis. POSSUM score includes 12 physiological and 6 operative variables in enumeration of morbidity and mortality [3] (Tables 1 and 2).
| Scores | ||||
|---|---|---|---|---|
| 1 | 2 | 4 | 8 | |
| Age ( in years ) | ≤ 60 | 61-70 | >71 | - |
| Cardiac signs Chest radiograph | No failure | Diuretic, digoxin, antianginal or hypertensive therapy | Peripheral edema; warfarin therapy borderline cardiomegaly | Raised jugular venous pressure cardiomegaly |
| Respiratory history Chest radiograph | No dyspnea | Dyspnea on exertion mild COAD | Limiting dyspnea (one flight) moderate COAD | Dyspnea at rest (rate >30/min) fibrosis or consolidation |
| Blood pressure systolic (mmHg) | 110-130 | 131-170 100-109 | 2171 90-99 | <89 |
| Pulse (beats/min) | 50-80 | 81-100 | 101-120 | >120 |
| Glasgow coma score | 15 | 12-14 | 9-11 | <9 |
| Hemoglobin (gm/100 ml) | 13-16 | 11.5-12.9 16.1-17.0 | 10.0-11.4 17.1-18.0 | <10 >18 |
| White cell count (× 1012/L) | 4-10 | 10.1-20.0 | 220.1 | - |
| Urea (mmol/L) | ≤ 7.5 | 7.6-10.0 | 10.1-15.0 | >15.1 |
| Sodium (mmol/L) | 2136 | 131-135 | 126-130 | <126 |
| Potassium (mmol /L) | 3.5-5.0 | 3.2-3.4 5.1-5.3 | 2.9-3.1 5.4-5.9 | <2.9 >5.9 |
| Electrocardiogram | Normal | - | Atrial fibrillation Rate (60 90/min) | Any other abnormal rhythm or 25 ectopic/min, Q waves or ST/T wave changes |
| Score | ||||
|---|---|---|---|---|
| 1 | 2 | 4 | 8 | |
| Operative severity* | Minor | Moderate | Major | Major+ |
| Multiple procedures | 1 | - | 2 | >2 |
| Total blood loss (in ml) | ≤ 100 | 101-500 | 501-999 | ≥ 1000 |
| Peritoneal soiling | None | Minimal (serous fluid) | Local pus | Bowel content, pus or blood |
| Presence of malignancy | None | Primary only | Nodal metastases | Distant metastases |
| Mode of surgery | Elective | - | Emergency resuscitation of >2 hours possible Operation <24 hours after admission | Emergency (immediate surgery<2 hours needed) |
POSSUM equation for morbidity
Ln R/1-R = (- 5.91+(0.16 × physiological score)+(0.19 × operative severity score)).
POSSUM equation for mortality
Ln R/1-R= (-7.04+(0.13 × physiological score)+(0.16 × operative severity score)).
Note: Where R is predicted risk.
Aims and objectives
- To assess the efficacy of modified POSSUM score in perforated peritonitis.
- To assess the efficacy of POSSUM scoring system in identifying risk factors for adverse outcome.
- To assess the efficacy of additional factor; time at presentation from onset of symptoms in predicting the post-operative outcome in patients with perforated peritonitis.
Methods
Prospective study conducted in patients presenting to patients presenting with peritonitis was evaluated with detailed history and clinical examination and pre-operative physiological variables and intra-operative variables were collected and the expected outcome was measured by using POSSUM equation. Patient was followed up for 4 week after the surgery. Outcome and complications were recorded.
- Type of study-Prospective.
- Duration of study-2 years (December 2020 to November 2022).
The study was conducted in the Department of Surgery, MVJ Medical College and Research Hospital, Hoskote from December 2020 to November 2022 (24 months). It was approved by the institute ethics committee. The study was a prospective observational of a single group of patients undergoing emergency laparotomy for hollow viscus perforation. All patients of established peritonitis following hollow viscus perforation were included in the study. Patients with primary peritonitis, peritonitis secondary to gynecological cause and peritonitis secondary to trauma were excluded from the study. The sample size was estimated using the sample size formula. A convenient sampling technique was followed.
Informed consent was obtained from patients. Patients presenting with peritonitis was evaluated with detailed history and clinical examination. Pre-operative physiological variables were collected. All patients underwent emergency laparotomy and operative variables were collected intra-operative. The expected outcome was measured by using POSSUM equation. Patient was followed up for 4 week after the surgery. Outcome and complications noted in patients were recorded.
Statistical analysis
The data was collected in individual patient proforma and was entered systematically in a Microsoft excel sheet (Redmond, WA, USA). Statistical analysis determined using Statistical Package for the Social Sciences (SPSS) 19.0 software (IBM Corp., Armonk, NY, USA). The data on categorical variables, such as gender and clinical characteristics were expressed as frequency and percentages. The normal distribution of data was tested using Kolmogorov-Smirnov (K-S) test. The expected mortality rate was obtained using linear regression analysis and the O:E ratio (Observed: Expected ratio) was calculated. Chi-square test applied to obtain the p value to note any significant difference between the predicted rate and the actual outcome. Rate of increment in complication for each risk factor was calculated based on the hypothesis and "t" test will apply to validate the hypothesis.
Results
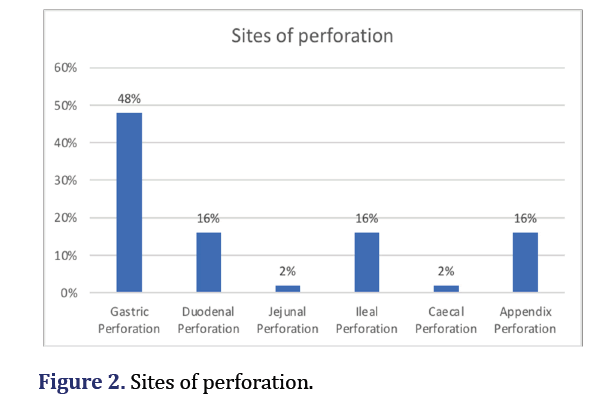
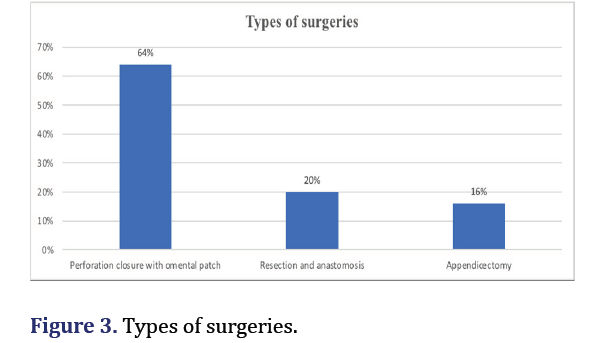
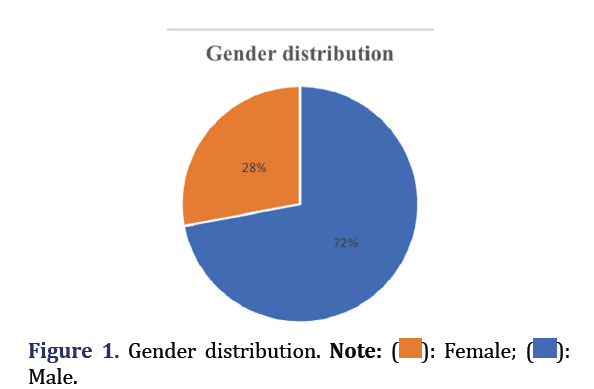
In our study there were a total of 50 patients, among them 36 were males and 14 were females. Most common site of perforation was gastric pre-pyloric perforation (48%) which include one patient of gastric malignancy presented as perforation. Other sites of perforation studied in our study were duodenal (16%), ileum (16%), appendix (16%), jejunum (2%) and caecum (2%). All cases were operated emergency which includes perforation closure with omental patch (64%), resection-anastomosis (20%) and appendicectomy (16%).
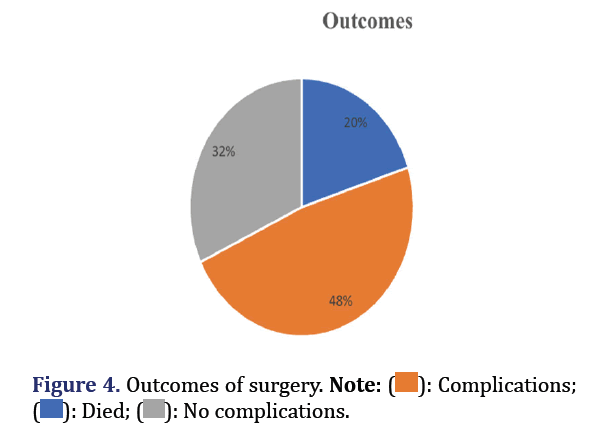
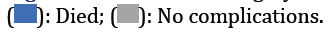
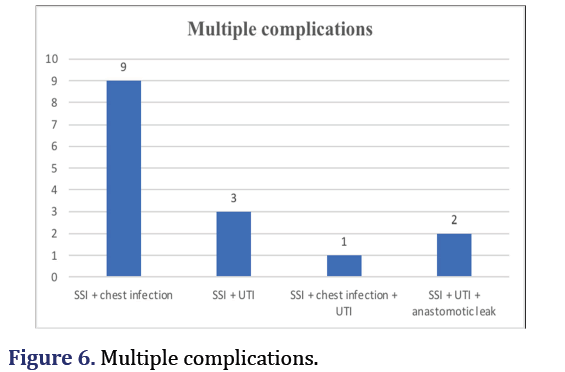
Out of 50 patients in our study, 10 patients died resulting in crude mortality rate of 20% and 24 patient developed complication in post-operative period, resulting in crude morbidity rate of 60%. The remaining 16 patients showed no evidence of any complication. Complications noted in our study were multiple complications (30%), surgical site infection (8%), septicaemia (6%) and chest infection (4%). Among patients with multiple complications, maximum number of patients presented with surgical site infection along with chest infection.
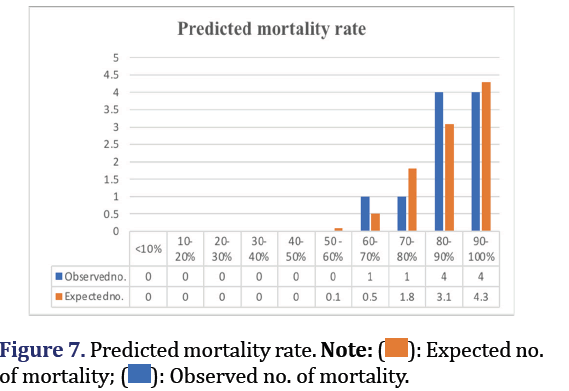
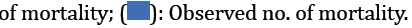
Using logistic equations, the predicted risk of mortality and morbidity was calculated and compared with the observed mortality and morbidity. An Observed to Expected ratio (O:E) for mortality was 1.020 (no significant difference) (p=0.980). An Observed to Expected ratio (O: E) for morbidity was 1.005 (no significant difference) (p=0.934). For mortality and morbidity, sensitivity was 80% and 97%, specificity was 95% and 93% and positive predictive value was 80% and 97%, negative predictive value was 95% and 93% respectively. Derived from logistics equation.
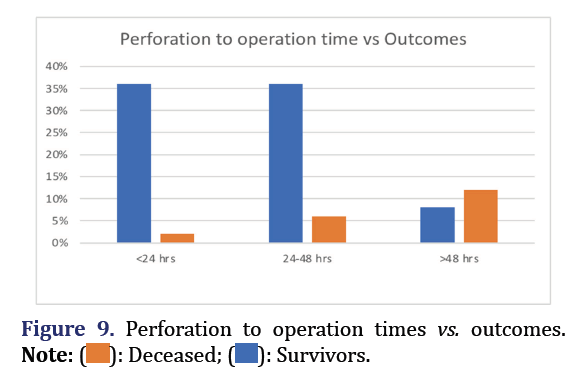
Analysis of POSSUM variables were obtained. Physiological variables such as cardiovascular system, blood pressure, hemoglobin, urea and serum potassium were found to be significant to cause adverse outcomes. Operative variables such as operative complexity, multiple procedure, presence of malignancy and mode of surgery were found to be significant to cause adverse outcomes. Additional factor-perforation to operation time was included in our study and showed more than 50% mortality if patient present late (>48 hrs) (Figures 1-9).
Discussion
Over the past few years, surgical audit has become more significant as a tool for evaluating the standard of surgical treatment and as a teaching tool. The use of the crude mortality rate in these days can be deceiving. Due to poverty and ignorance, a particular illness's presentation is delayed in a developing country like India, which causes more complications and higher death rates. There have been many scoring systems developed, including the American Society of Anesthesiologists (ASA) for general risk prediction, Acute Physiology and Chronic Health Evaluation III (APACHE III) for intensive care and the Goldman Index for cardiac-related problems after surgery [4-7].
The POSSUM score method can be used to identify patients with perforated peritonitis who have a higher risk of mortality or complications. POSSUM was developed by Copeland et al. from a cohort of 1372 patients in 1991 mainly for surgical audits [3]. It is a scoring system based on 12 pre-operative physiological factors and six operative factors [3]. Each factor is scored with 4 graded score values; the sum of individual scores was used to predict post-operative outcome.
In our study there were a total of 50 patients studied, among them 36 were males and 14 were females. Similar studies which shows male preponderance were Chatterjee et al. (88%), Gurjar et al. (68.5%), Batra et al. (88%) and Manivannan et al. (87%) [8-11].
Most common indication of surgery was gastric pre-pyloric perforations (48%) which include one patient of gastric malignancy presented as perforation. Other sites of perforation studied in our study were duodenal (16%), ileum (16%), appendix (16%), jejunum (2%) and caecum (2%). Gurjar et al. [9] and Murugappan et al. [12] obtained similar results which showed 53% patients and 58% presented with gastric pre-pyloric perforation respectively. A study by Batra et al. [10] (80%) and Manikanta et al. [13] (66%) shows gastro-duodenal perforation as a most common site of gastrointestinal perforation. However studies by Manivannan et al. [11] and Kumar et al. [14] and report that Duodenal perforation is most common site of perforation in gastrointestinal tract. All the patients underwent emergency surgery which includes perforation closure with omental patch (64%), resection-anastomosis (20%) and appendicectomy (16%).
In our study, death occurred in 10 patients out of 50 patients resulting in crude mortality rate of 20% and out of remaining 40 patients, 24 patients developed complications resulting in crude morbidity rate of 60%. Gurjar et al. [9] reported crude mortality rate of 17.40%, Kumar et al. [14] reported mortality rate of 18%, Chatterjee et al. [8] reported mortality rate of 18%. However few studies reported lesser mortality rate, Batra et al. [10] (5.70%), Manivannan et al. [11] (4%) and Manikanta et al. [13] (5.7%).
Complications noted in our study were chest infection (4%), surgical site infection (8%), septicemia (6%) and multiple complications (30%). Kumar et al. [14] obtained similar results which shows 30% patients developed multiple complications in post-operative period. However wound infection reported to be commonest complication in studies by Gurjar et al. [9], Manivannan et al. [11], Murugappan et al. [12], Manikanta et al. [13].
In our study, maximum number of patients presented late >24 hrs (66%) which corresponds well with other studies such as Chatterjee et al. [8] (62%) and Batra et al. [10] (66.20%). In our study, analysis of risk factors were done, factors such as cardiovascular system, blood pressure, hemoglobin, blood urea, serum potassium, operative complexity, multiple procedure, presence of malignancy, mode of surgery were found to be significant. Additional factor perforation to operation time was included in our study and found to be significant.
Comparison of observed and POSSUM predicted mortality rates and morbidity rates were done using linear analysis. An Observed to Expected ratio (O:E) for mortality was 1.020 (there was no significant difference between the predicted and observed values), (p=0.980) and for morbidity was 0.997 (there was no significant difference between the predicted and observed values), (p=0.893). Chatterjee et al. [8] noted the similar results of O:E ratio of mortality and morbidity was 1.005 and 1.001 respectively and same results obtained by Kumar et al. [14] O:E ratio of mortality and morbidity to be 1.005 and 1.001 respectively. Vishwani et al. [15] found that POSSUM scoring system is reasonably good predictor of mortality (O:E=0.6) and morbidity (O:E=0.7) using exponential and linear analysis respectively. Similar finding was obtained by Prytherach et al. (O:E=0.9) [16], Sagar et al. (O:E=0.87) [17] and Parihar et al. (O:E=0.97) [18] (Table 3).
| Studies | Male preponderance | Commones t site of perforation | Commones t complications | Mortality rate | O:E ratio for mortality | O:E ratio for morbidity | Reference number |
|---|---|---|---|---|---|---|---|
| Present study | 72% | Pre-pylorie (gastric) 48% | Multiple infections 30% | 20% | 1.02 | 0.997 | |
| Chatterjee et al. | 88% | - | - | 18% | 1.005 | 1.001 | [8] |
| Gurjar et al. | 68.50% | Pre-pylorie (gastric) 53% | Wound infection | 17.40% | - | - | [9] |
| Batra et al. | 88% | Gastro-duo denal 80% | Fever | 5.70% | - | - | [10] |
| Manivannan et al. | 87% | Duodenal 75% | Wound dehiscence | 4% | - | - | [11] |
| Murugappan et al. | 88.50% | Pre-pylorie (gastric) 58% | Wound infection | - | - | - | [12] |
| Manikanta et al. | - | Gastro-duo denal 66% | Wound infection | 5.70% | - | - | [13] |
| Kumar et al. | - | Duodenal 48% | Multiple infections 30% | 18% | 1.005 | 1.001 | [14] |
| Vishwani et al. | - | - | - | - | 0.6 | 0.7 | [15] |
| Pyrtherach et al. | - | - | - | - | 0.9 | - | [16] |
| Sagar et al. | - | - | - | - | 0.87 | - | [17] |
| Parihar et al. | - | - | - | - | 0.97 | - | [18] |
Conclusion
POSSUM scoring system is better since it’s include both physiological and operative parameters and can be used as a significant tool for predicting outcomes in perforated peritonitis. Depends on the scoring system, patients attender can be counseled pre-operatively and prior correction of risk factors can be done. Strict vigilance and prompt adjustment of the verified parameters can improve the patient's overall health and decrease morbidity and mortality. Widespread awareness and education about perforated peritonitis, early referrals, early diagnosis and prompt treatment must be implemented to shorten the duration of perforation to operation time.
Acknowledgements
I want to acknowledge the efforts taken by the entire team for working hard towards this article.
Declarations
Ethical approval
Ethical approval was obtained from institute of ethical committee.
Funding
No funding sources.
Conflict of interest
None declared.
References
- Zinner MJ, Ashley SW. Maingot’s abdominal operations. 12th edn, USA. 1997:1159-1172.
- Hospital WMU. Clinical Audit. Middlesex: West Middlesex University Hospital; 2010.
- Copeland GP, Jones D, Walters MP. POSSUM: A scoring system for surgical audit. Br J Surg 1991;78(3):355-360.
[Crossref] [Google Scholar] [Pubmed]
- Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system: Risk prediction of hospital mortality for critically III hospitalized adults. Chest 1991;100(6):1619-1636.
[Crossref] [Google Scholar] [Pubmed]
- Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297(16):845-850.
[Crossref] [Google Scholar] [Pubmed]
- Tekkis PP, Prytherch DR, Kocher HM, Senapati A, Poloniecki JD, Stamatakis JD, et al. Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg 2004;91(9):1174-1182.
[Crossref] [Google Scholar] [Pubmed]
- Tekkis PP, Poloniecki JD, Thompson MR, Stamatakis JD. Operative mortality in colorectal cancer: Prospective national study. BMJ 2003;327(7425):1196-1201.
[Crossref] [Google Scholar] [Pubmed]
- Chatterjee AS, Renganathan DN. POSSUM: A scoring system for perforative peritonitis. J Clin Diagn Res 2015;9(4):PC05.
[Crossref] [Google Scholar] [Pubmed]
- Sunil G, Suraj J, Abhishek K, Advait P. Study of POSSUM score for risk assessment in patients of perforation peritonitis at a tertiary care teaching hospital. Int J Health Clin Res 2021;4(9): 99–105.
- Batra P, Batra R, Utaal MS. POSSUM scoring system for predicting prognosis in patients of perforation peritonitis. Int Surg J 2016;3(4):2115-2119.
- Nachiappan M, Litake MM. Scoring systems for outcome prediction of patients with perforation peritonitis. J Clin Diagn Res 2016;10(3):PC01-PC05.
[Crossref] [Google Scholar] [Pubmed]
- Dhanraj M, Murugan P, Duraisami V, Rengan V. Evaluation of POSSUM scoring in patients undergoing emergency laparotomy for hollow viscus perforation. Int Arch Integrate Med 2018;5(5):21-26.
- Manikanta KS, Sharangouda CP, NoorUl H. A clinical study of prognostic factors in typhoid ileal perforation: In a tertiary hospital. SSRG Int J Med Sci 2016;3(5):1-10.
[Crossref]
- Kumar A, Suman S, Kundan K, Kumar P. Evaluation of POSSUM scoring system in patients with perforation peritonitis. Int Surg J 2016;3(4):2181-2186.
- Vishwani A, Gaikwad VV, Kulkarni RM, Murchite S. Efficacy of POSSUM scoring system in predicting mortality and morbidity in patients of peritonitis undergoing laparotomy. Int J Sci Stud 2014;2(4):29-36.
- Prytherch DR, Whiteley MS, Higgins B, Weaver PC, Prout WG, Powell SJ, et al. POSSUM and portsmouth POSSUM for predicting mortality. Bri J Surg 1998;85(9):1217-1220.
[Crossref] [Google Scholar] [Pubmed]
- Sagar PM, Hartley MN, MacFie J, Taylor BA, Copeland GP. Comparison of individual surgeon's performance: Risk-adjusted analysis with POSSUM scoring system. Dis Colon Rectum 1996;39(6):654-658.
[Crossref] [Google Scholar] [Pubmed]
- Parihar V, Sharma D, Kohli R, Sharma DB. Risk adjustment for audit of low risk general surgical patients by Jabalpur-POSSUM score. Indian J Surg 2005;67(1):38-42.








 Male.
Male.