Research Article - Archives of Clinical and Experimental Surgery (2022)
Outcomes of Gastrointestinal Fistulas: Results from a Multi-Continent, Multi-National Multi-Center Cohort
Humberto Arenas Marquez*, Maria Isabel Turcios Correia, Juan Francisco Gracia, Roberto Anaya Prado, Arturo Vergara, Jorge Luis Garnica, Alejandra Cacho, Miguel Mendoza Navarrete and Sergio Santana PorbanHumberto Arenas Marquez, San Javier Hospital, Jalisco, Mexico, Email: arenas50@hotmail.com
Received: 15-Dec-2021, Manuscript No. EJMACES-22-48001; Editor assigned: 17-Dec-2021, Pre QC No. EJMACES-22-48001 (PQ); Reviewed: 31-Dec-2021, QC No. EJMACES-22-48001; Revised: 05-Jan-2022, Manuscript No. EJMACES-22-48001 (R); Published: 12-Jan-2022
Abstract
Rationale: Gastro Intestinal Fistulas (GIF) represents a severe and potentially lethal complication of the hospital surgical activity. However, evidences are lacking about prognosis and outcomes of GIF in Latin America (LATAM) hospitals.
Objective: To describe the prognosis and outcomes GIF in LATAM hospitals
Study design: Prospective, longitudinal, cohort-type study. The cohort fostered three cross-sectional examinations: 1st examination: On admission of the patient in the study; 2nd examination: Thirty days later; and 3rd (and last) examination: Sixty days after patient´s admission.
Study serie: One hundred seventy-seven patients (Males: 58.2%; Average age: 51.0 ± 16.7 years; Ages ≥ 60 years: 36.2%) diagnosed with, and assisted for, GIF (ECF: Enterocutaneous: 64.9% vs. EAF: Enteroathmospheric: 35.1%) in 76 LATAM hospitals (13 countries) and Europe (4).
Methods: Condition (alive vs. deceased) and hospital status (hospitalized vs. discharged) of the patient, and the GFI patency (closed vs. non closed) were recorded in each of the cohort´s examination. Indicators of GFI prognosis thus constructed were correlated with demographical, sanitary, surgical and nutritional characteristics of the patients.
Results: On conclusion of the study indicators of GIF prognosis behaved as follows: Mortality: 14.7%; Prolonged hospitalization: 47.4%; Spontaneous closure of GIF: 36.2%. Type of GIF influenced upon patient´s survival: ECF: 87.0% vs. EAF: 82.3% (Δ=+4.7%; χ2=6.787; p<0.05). In each examination of the cohort, the number of surviving subjects was always greater among those with ECF: After 30 days: ECF: 92.1% vs. EAF: 83.9% (Δ=+8.2%); after 60 days: ECF: 98.1% vs. EAF: 90.4 % (Δ=+7.7%;χ22=13.764; p<0.05). On the other hand, hospital stay was prolonged in the subjects of elective surgery (Elective surgery: 61.4% vs. Emergency surgery: 38.3% (Δ=+23.1%; Δ2=9.064; p<0.05) and those with a reduced calf circumference (χ2=12.655; p<0.05). Location of the fistula also influenced upon prolongation of hospital stay (χ2=7.817; p< 0.05).
Conclusions: Type of GIF influences upon survival of the patient. On the hand, hospital stay was dependent upon type of surgery previously performed, location of the fistula, and calf circumference value on admission in the study serie.
Introduction
Gastro Intestinal Fistulas (GIF) represent a serious complication of the surgical processes, and bear a high risk of hydro electrolyte disorders, sepsis, malnutrition and death [1,2]. Hence, with repercussions of GIF known, timely recognition, accurate diagnosis (integrating criteria on the spontaneous closure also read as conservative (non-surgical- of the GIF); and adoption of the required measures for hydro electrolyte repletion, nutritional support and containment of sepsis are imperative for a better prognosis of GIF.
Incidence of GIF is estimated to vary between 4%- 20% of the operated patients, but this estimate might vary with the typology of the health institution, and the volume and complexity of the surgeries completed in a year. Almost half of the GIF originate in patients in whom no intestinal anastomosis is performed, but suffer inadvertent enterectomies during the surgical act [3,4]. The other half of GIF is caused by disruption (partial or complete) of the intestinal suture made. Reoperations with extensive lysis of adhesions and adherences, laparoscopic surgery, reparation of ventral hernias, tumor cytoreduction, and trauma inflicted during surgery not related with tumor cytoreduction are among the surgical procedures commonly associated with postsurgical GIF [3,4]. GIF-related mortality could be as high as 80% of the affected patients [3,4]. It is then immediate that management of GIF leads to prolonged hospitalizations, a higher quota of clinical and surgical actions, and increased health care costs.
Management and resolution of GIF have called the attention of groups of experts and professional societies alike. In this regard, the “ASPEN/FELANPE clinical guidelines for nutrition support of adult patients with enterocutaneous fistula” are to be mentioned [5,6]. Identification of the origin of the fistula, containment of surgical damage, and exteriorization of the fistula leakage might be actions initially recommended. Further actions in the management of GIF might imply the better assessment on their likely spontaneous closure. It is worthy to note coming to this point in the present narrative Crohn disease, malignancies of the Gastro Intestinal Tract (GIT), and a hostile abdomen due to adherences, adhesions and reinterventions are always mentioned as negative predictors of the spontaneous closure of the fistula.
There are previous studies on the prevalence of GIF in hospitals of Latin America (LATAM), and practices adopted by the surgical care teams for the management and resolution of GIF. For the same reason, there are no estimates of the current effectiveness of different management guidelines that could be followed for GIF resolution.
The goals previously exposed might be achieved through “research outcomes” type studies reuniting data generated by the surgical care teams managing GIF locally in order to show the current state of therapeutic effectiveness, to identify those actions leading to an unsatisfactory evolution of both the fistula and the patient, and, for the same reason, to find those teams distinguishing themselves for a higher therapeutic effectiveness for exploring the conducted practices, and validate and disseminate them to the others. Regarding this issue, the “Consenso Mexicano para el Tratamiento Integral de las Fistulas Digestivas” (first published 21 years ago) suggested the development, implementation and management of a national registry reuniting those variables that could be associated with adverse events during GIF management in order to correct inadequate practices and at the same improve quality of treatment[7]. Recent advances in information and communication technologies have provided researchers with sophisticated tools for building and managing large databases and analyzing massive amounts of data, all of them eventually leading to a better treatment of GIF.
Given the aforementioned, the Federación Latinoamericana de Terapia Nutricional, Nutrición Clínica y Metabolismo has launched the “Fistula Day” Project as a multi-center, multi-national effort having as supraobjective the drafting and validation of the “Good Practices” in the management of GIF. Such supraobjective will be met by means of regular surveys among LATAM institutions dedicated to GIF management, and collection of relevant data on the clinical characteristics of the GIF patients, locally conducted practices, and results observed at the moment of the survey. With this purpose, FELANPE has commissioned the SANVITE Unit for Intestine Failure at “San Javier” Hospital (Guadalajara, Estado de Jalisco, México) for the design, conduction and management of activities revealing the current surgical treatment of GIF, the effectiveness of such treatments, and the nutritional care provided to the GIF patient as part of such treatments.
Presentation of the Fistula Day Project (FDP)
The “Fistula Day” is a research outcome-type project oriented to the construction of a map with the diagnosis, treatment and resolution of GIF in LATAM hospitals. As such, the “Fistula Day” foresees the completion of cross-sectional surveys at regular intervals among LATAM hospitals in order to obtain estimates of the operational characteristics of the hospitals treating GIF patients on one hand; and the demographic, sanitary, clinical-surgical and nutritional characteristics of the patients on the other; as well as the surgical practices conducted in them for intervening the surgical damage, and the nutritional support schemes currently administered to the patient as part of the resolution of GIF.
Integrating the results of the cross-sectional surveys completed as part of the “Fistula Day” into a cohort will also serve to assess the impact of findings and practices revealed upon 3 outcomes of interest for researchers: survival of the patient, prolongation of the hospital stay, and the spontaneous closure of the fistula. Eventually, the “Fistula Day” will provide the methodological and operational foundation for assessing the impact of the “Good Practices” ultimately adopted in the diagnosis, treatment and follow-up of GIF.
The design of the “Fistula Day” will be presented in this report, along with the demographical, sanitary, surgical and nutritional characteristics of the patients admitted in the first cohort, and the associations found with the indicators of prognosis and outcomes of GIF at the end of the research. Influence of the characteristics of the participating hospitals upon prognosis and outcomes of GIF will be addressed in an accompanying paper.
Materials and Methods
Study design
Prospective, multi-national, multi-center cohort-type study. The design of the study foresaw 3 cross-sectional examinations in different times: 0, 30 and 60 days. Admission of the hospitals participating in the “Fistula Day” was completed on the first examination (Day 0). Successive examinations at 30 and 60 days were made for documenting the evolution of the patient, surgical practices performed, therapeutic response, and nutritional care administered.
Inclusion criteria
Adult’s patients diagnosed and treated for GIF in second and third-level LATAM hospitals. GIF was established after output of intestinal liquor through an orifice in the abdominal wall and/or the exposure of the intestinal mucosae to the exterior [1-6]. Exclusion criteria: Patients with fistulas of the biliary tree and the pancreatic duct were excluded.
Methods
LATAM medical centers dedicated to the treatment of GIF were invited to participate in the “Fistula Day” through communications made by the societies, associations and colleges represented in FELANPE, notifications issued through social networks, and direct electronic messages. A web page was open for registering the participating center, downloading and management of “Fistula Day” tools and resources, and communication and interaction between researchers and participating centers.
As previously mentioned, the design of “Fistula Day” comprised 3 cross-sectional examinations. The first examination was completed on May 9th, 2018 with the registry of participating hospitals, and the collection of their sanitary and managerial characteristics. Once admission of the hospital in the “Fistula Day” was completed, patients locally assisted for GIF, and their demographical, clinical, surgical and nutritional characteristics were then entered into the forms provided by the design of the research. Current practices related with the surgical treatment of GIF, along with implemented nutritional support schemes, were also recorded.
Forms with data collected during the first examination were submitted by electronic mail to the coordinator center of the “Fistula Day” as proof of participation. Similarly, data collected in this first examination were locally entered into an on-line application built with Red Cap (University of Vanderbilt, United States).
The other two surveys contemplated in the “Fistula Day” project were completed at 30 days (June 9th 2018) and 60 days (July 9th, 2018) after the first one in order to record the evolution of the patient, and the therapeutic response achieved. No new cases were admitted in the subsequent “Fistula Day” examinations.
Data processing and statistical-mathematical analysis of the results
R program for statistical management and analysis (R Core Team 2018 version 3.5.0, United States) was used for debugging, preparing and processing data collected during the “Fistula Day” surveys. Data were reduced to absolute/relative frequencies and percentages regarding variable type and the objective of statistical analysis.
Condition of the patient (Alive/Deceased), hospital stay (Prolonged/Discharged) and spontaneous closure (Yes/No) of the fistula were assumed as 30 and 60 days outcomes of the “Fistula Day”. Nature and strength of the associations between the results of the “Fistula Day”, on one hand, and the characteristics of hospitals and patients included in the cohort, on the other, were examined with appropriate statistical tests regarding the variable type. Existent differences between cohorts of patients according with the selected predictor were evaluated with the log-rank test based on the chi- square distribution [8]. A level lower than 5% was used in all the instances for denoting the finding as significant.
Treatment of missing data
Data lost during follow-up of the patient were replaced with the observation entered in the preceding examination according with the LOCF (for “Last Observation Carried Forward”) method.
Intention-to-treat
Data collected during the “Fistula Day” were analyzed according with the “Intention to treat” principle in order to keep the size of the cohort constant in each of the surveys foreseen in the cohort [9].
Ethical considerations
The protocol followed by local surveyors during the “Fistula Day” was drafted according with “Good Clinical Practices” [10]. Identity and rights of the surveyed patients were also protected [11]. The patients (and by extension their caretakers) were informed about the purposes of the research, and the non-invasive nature of the procedures. Collected data were adequately preserved in order to ensure anonymity and confidentiality. Aggregated data were used in the interpretation of the results and the realization of statistical inferences. Informed consent was obtained from the patient before inclusion in the cohort. Local conduction of the activities foreseen in the “Fistula Day” was authorized and supervised by the hospital Committees of Ethics after presentation, review and approval of the research protocols.
The researchers entrusted with the conduction of the “Fistula Day Project” presented the protocol “Current status of the postoperative fistula of digestive tract; multicentric, multinational study. DAY OF THE FISTULA” before the Ethics Committee of the San Javier Hospital (city of Guadalajara, State of Jalisco, México) for review and approval. A ruling was emitted on April 11th, 2018 by Dr. Eduardo Razón Gutiérrez, acting Director of the Ethics Committee, with the approval of the research protocol and the authorization for the conduction of the “Fistula Day” Project.
Results
At the conclusion of the first “Fistula Day” examination 177 patients diagnosed with, and treated for, GIF in 76 hospitals of LATAM (13 countries) and Europe (4) were admitted. The presence of patients attended in non-LATAM hospitals corresponded with the medical care teams` desires to be included in the study cohort and sharing the locally collected data. However, non-LATAM patients amounted less than 10% of the size of the cohort. On the other hand, half plus one of the patients admitted in the cohort were Mexicans.
Influence of the demographical, clinical and sanitary characteristics of the patients upon prognosis and outcomes of GIF
Table 1 shows demographical, clinical and sanitary characteristics of the patients finally included in the “Fistula Day” study serie. Men prevailed over women (Males: 58.2% of the study serie). Average age was 51.0 ± 16.7 years. Subjects with age’s ≥ 60 years were 36.2% of the studied cases. Fifty-nine-point-six percent of the patients accumulated between 0-30 days of hospital stay on admission into the study serie. A cancer diagnosis was made in 27.7% of the patients (Table 1).
| Characteristic | Findings |
|---|---|
| Sex | Males: 103 [58.2] |
| Females: 74 [41.8] | |
| Age, years, mean ± standard deviation | 51.0 ± 16.7 |
| Age, years | <60 years: 113 [63.8] |
| ≥ 60 years: 64 [36.2] | |
| Country/region of origin | European countries: 17 [ 9.6] |
| Latin America: 160 [90.4] | |
| México: 96 | |
| Other Latin-American countries: 64 | |
| Hospital stay | Between 0-30 days: 105 [59.3] |
| Between 30-60 days: 45 [25.4] | |
| +60 days: 27 [15.3] | |
| Cancer | Present: 49 [27.7] |
| Absent: 128 [76.3] | |
| Source: Records of the study. Size of the serie: 177. | |
On the closure of the “Fistula Day” window of observation, 26 deaths were registered (14.7% of the size of the cohort) along with 84 prolonged hospitalizations (47.4%). Spontaneous closure of the GIF was reported in 64 (36.1%) of the examined patients. Table 2 shows the 30- and 60-days “Fistula Day” outcomes. Twenty patients (11.3% of the size of the cohort) were lost to follow-up. In spite of this, estimates of the indicators of prognosis and outcomes of GIF were independent from the method of analysis used (Table 2).
| Moment | 30 days follow-up | 60 days follow-up | ||
|---|---|---|---|---|
| Method of analysis | Intention-to-treat | Analysis-per-protocol | Intention-to-treat | Analysis-per-protocol |
| Size of the serie | ||||
| Expected | 177 | 165 | 177 | 157 |
| Lost to follow-up | 12 | 20 | ||
| Condition of the paient | ||||
| Alive | 158 [89.3] | 146 [88.5] | 151 [85.3] | 131 [83.4] |
| Deceased | 19 [10.7] | 19 [11.5] | 26 [14.7] | 26 [16.6] |
| Hospitalized | 63 | 63 | 84 | 84 |
| [35.6] | [38.2] | [47.4] | [53.5] | |
| Spontaneous closure | 60 | 60 | 64 | 64 |
| [33.9] | [36.4] | [36.2] | [40.8] | |
| Source: Records of the study. Size of the serie: 177 | ||||
Table 3 shows the associations between demographical, clinical and sanitary characteristics of the patients and the indicators of the study’s outcomes. As shown, study’s results were independent from the demographical, clinical and sanitary characteristics of the patients (Table 3).
| Characteristic | Findings | Interpretation |
|---|---|---|
| Survival of the patient | ||
| Sex of the patient | Male: 87.4 | χ2=0.841 |
| Female: 82.4 | ||
| Age of the patient | <60 years: 85.0 | χ2=0.031 |
| ≥ 60 years: 85.9 | ||
| Diagnosis of cancer | Present: 87.8 | χ2=0.323 |
| Absent: 84.4 | ||
| Previous hospital stay | 0-30 days: 81.9 | χ2=3.283 |
| 31-60 days: 94.3 | ||
| >60 days: 85.2 | ||
| Prolonged hospitalization | ||
| Sex of the patient | Male: 50.5 | χ2=0.906 |
| Female: 43.2 | ||
| Age of the patient | <60 years: 52.2 | χ2=2.833 |
| ≥ 60 years: 39.1 | ||
| Diagnosis of cancer | Present: 55.1 | χ2=1.538 |
| Absent: 44.5 | ||
| Previous hospital stay | 0-30 days: 50.5 | χ2=0.977 |
| 31-60 days: 42.2 | ||
| >60 days: 44.4 | ||
| Spontaneous closure of the fistula | ||
| Sex of the patient | Masculino: 39.8 | χ2=1.420 |
| Femenino: 31.1 | ||
| Age of the patient | <60 years: 34.5 | χ2=0.366 |
| ≥ 60 years: 39.1 | ||
| Diagnosis of cancer | Present: 36.7 | χ2= 0.009 |
| Absent: 35.9 | ||
| Previous hospital stay | 0-30 days: 34.3 | χ2=0.969 |
| 31-60 days: 42.2 | ||
| >60 days: 33.3 | ||
| Source: Records of the study. Size of the serie: 177 | ||
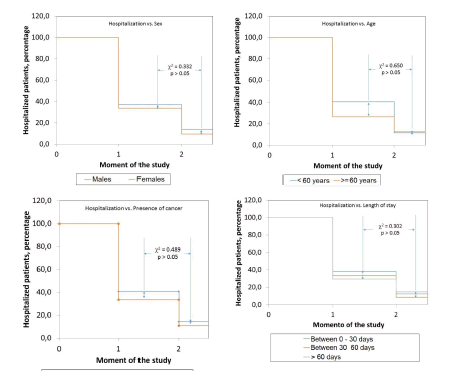
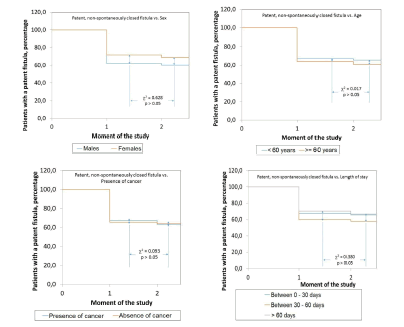
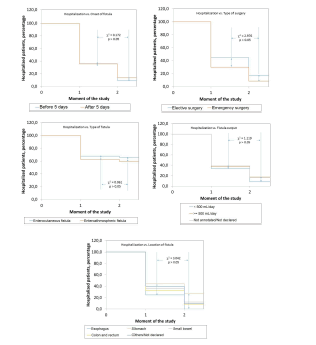
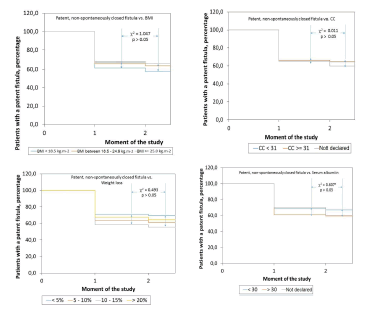
Figures 1-3 show the behavior of the cohort as disaggregated regarding the demographical, clinical and sanitary characteristics of the studied patients in order to assess the prognosis and outcomes of GIF. As shown, behavior of the cohort in each case was independent from the demographical, clinical and sanitary characteristics of the studied patients (Figures 1-3).
Influence of the characteristics of the gastrointestinal fistulas upon prognosis and outcomes of the fistula
Figure 3. Behavior of the spontaneous closure of gastrointestinal fistulas in the patients included in the cohort according with the demographical, clinical and sanitary characteristics as documented on admission in the “Fistula Day” project. Curves were constructed with patients with a patent, non-spontaneously closed fistula, in the corresponding moment of the study.
Table 4 shows the characteristics of the GIF documented in this study. Patients with ECF prevailed. Almost 60% of the GIF showed an output <500 mL/day. Small bowel and colon were the predominant locations as source of the GIF. Half plus one of the GIF was diagnosed after elapsing the first 5 days of the primary surgery. In addition, 60.5% of the GIF originated after an emergency surgery. It is to be noticed that a bariatric surgery was completed in less than 4% of the studied patients (Table 4).
|
Characteristics of the fistulas |
Findings |
|
Fistulas diagnosed after |
During the first 5 days after surgery: 84 [47.5] |
|
5 days after surgery: 93 [52.5] |
|
|
Type of primary surgery |
Elective surgery: 70 [39.5] |
|
Emergency surgery: 107 [60.5] |
|
|
Nature of the fistula |
Enterocutaneous fistulas: 115 [64.9] |
|
Enteroathmosperic fistulas: 62 [35.1] |
|
|
Location of the fistula
|
Esophagus: 12 [ 6.8] |
|
Stomach: 18 [10.2] |
|
|
Small bowel: 88 [49.7] |
|
|
Colon and rectum: 49 [27.7] |
|
|
Other locations/No declared: 10 [ 5.6] |
|
|
Output of the fistula
|
Low: <500 mL/24 hours: 106 [59.9] |
|
High: ≥ 500 mL/24 hours: 40 [22.6] |
|
|
No output/No declared: 31 [17.5] |
|
|
Source: Records of the study. Size of the serie: 177. |
|
Table 5 shows the associations between GIF characteristics and the outcomes indicators of the study. Type of GIF influenced upon 60-days survival (and mortality as a complementary finding) of the patient: survival of the patient was lower among patients with an EAF: EAF: 82.3% vs. ECF: 87.0% (Δ=-4.7% χ2=6.878; p<0.05). Type of surgery previously performed also influenced upon prolongation of hospital stay: Elective surgery: 61.4% vs. Emergency surgery: 38.3 % (Δ=+23.1%; χ2=9.064; p<0.05) (Table 5).
|
Characteristic |
Findings |
Interpretation |
|---|---|---|
|
Survival of the patient |
||
|
Onset of the fistula |
Before 5 days: 84.5 |
χ2=0.079 |
|
After 5 days: 86.0 |
||
|
Type of surgery |
Elective surgery: 84.3 |
χ2=0.09 |
|
Emergency surgery: 85.9 |
||
|
Type of fistula |
ECF: 87.0 |
χ2=6.878 |
|
EAF: 82.3 |
|
|
|
Fistula output
|
<500 mL/24 hours: 89.6 |
χ2=4.013
|
|
>500 mL/24 hours: 80.0 |
||
|
Not recorded/Not declared: 77.4 |
||
|
Location of the fistula
|
Esophagus: 91.7 |
χ2=1.006
|
|
Stomach: 86.3 |
||
|
Small bowel: 84.1 |
||
|
Colon and rectum: 87.8 |
||
|
Other locations/Not declared: 80.0 |
||
|
Prolonged hospitalization |
||
|
Onset of the fistula |
Before 5 days: 45.2 |
χ2=0.315 |
|
After 5 days: 10.7 |
||
|
Type of surgery |
Elective surgery: 61.7 |
χ2=9.064 |
|
Emergency surgery: 38.3 |
||
|
Type of fistula |
ECF: 46.1 |
χ2=0.247 |
|
EAF: 50.0 |
||
|
Fistula output
|
<500 mL/24 hours: 42.5 |
χ2=2.655
|
|
>500 mL/24 hours: 55.0 |
||
|
Not recorded/Not declared: 54.8 |
||
|
Location of the fistula
|
Esophagus: 25.0 |
χ2=7.817
|
|
Stomach: 72.2 |
||
|
Small bowel: 48.9 |
||
|
Colon and rectum: 40.8 |
||
|
Other locations/Not declared: 50.0 |
||
|
Spontaneous closure |
||
|
Onset of the fistula |
Before 5 days: 39.3 |
χ2=0.677 |
|
After 5 days: 33.3 |
||
|
Type of surgery |
Elective surgery: 30.0 |
χ2=1.902 |
|
Emergency surgery: 40.2 |
||
|
Type of fistula |
ECF: 33.9 |
χ2=0.717 |
|
EAF: 40.3 |
||
|
Fistula output
|
<500 mL/24 hours: 35.9 |
χ2=0.041
|
|
>500 mL/24 hours: 37.5 |
||
|
Not recorded/Not declared: 35.5 |
||
|
Location of the fistula
|
Esophagus: 41.7 |
χ2=2.466
|
|
Stomach: 33.3 |
||
|
Small bowel: 34.1 |
||
|
Colon and rectum: 42.9 |
||
|
Other locations/Not declared: 20.0 |
||
|
p<0.05. Source: Records of the study. Size of the serie: 177. |
||
Similarly, influence of the location of the fistula upon prolongation of the hospitalization is to be signaled: patients with a fistula originated in the stomach (72.2% of those within this location), small bowel (48.9%), and colon and rectum (48.1%) exhibited the highest rates of prolonged hospitalization (Δ2=7.817; p<0.05). However, uneven distribution of the different locations of GIF should not be overlooked; a common finding in observational studies.
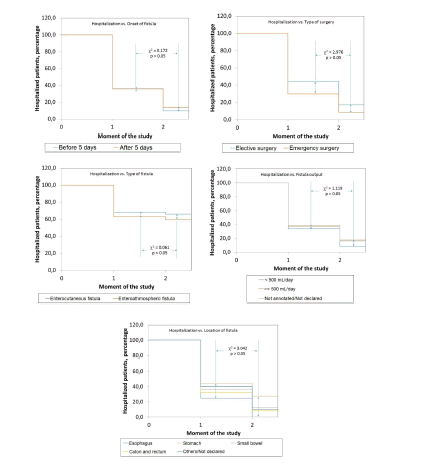
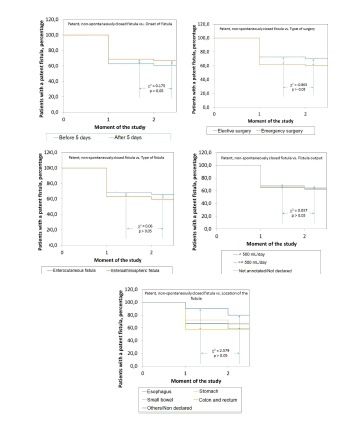
Figures 4-6 show the influence of the GIF characteristics upon the behavior of the cohort. Only the type of GIF influenced upon survival of the patient: the number of surviving subjects was always among those with an ECF: At 30 days: ECF: 92.1% vs. EAF: 83.9% (Δ=+8.2%); at 60 days: ECF: 98.1% vs. EAF: 90.4% (Δ=+7.7%; χ2=13.764; p<0.05). On the contrary, cohorts of patients disaggregated regarding type of previous surgery did not differ between them: At 30 days: Elective surgery: 44.3% vs. Emergency surgery: 29.9% (Δ=+14.4%); at 60 days: Elective surgery: 30.8% vs.Emergency surgery: 12.0% (Δ=+18.8%; χ2=2.975; p=0.0845). Cohorts of patients disaggregated according with location of fistula did not differ between them either (χ2=3.042; p>0.05) (Figures 4-6).
Figure 6. Behavior of the spontaneous closure of gastrointestinal fistulas in the patients included in the cohort according with the characteristics of the fistulas as documented on admission in the “Fistula Day” project. Curves were constructed with patients with a patent, non-spontaneously closed fistula, in the corresponding moment of the study.
Influence of the nutritional status of the patient
Table 6 shows the nutritional characteristics of the GIF patients. Average BMI was 24.3 ± 6.1 kg.m-2. Excessive body weight presented in 40.1% of the cases. However, more than a third of the GIF patients referred weight loss>10% on admission in the study. Average Calf Circumference (CC) was 30.5 ± 16.9 cm. half plus one of the patients presented with a CC<31 cm: cut-off point used in the description of this indicator. It is to be noticed that CC was not measured in the tenth of the GIF patients. More than half of the GIF patients had a serum albumin<30 g.L-1. Only 52.5% of the C reactive protein (PCR) determinations were recovered: the reason foe excluding this nutritional indicator from the analyses (Table 6).
|
Characteristic |
Findings |
|---|---|
|
Height, cm |
164.6 ± 9.3 |
|
Body weight, kg |
66.0 ± 17.6 |
|
Body Mass Index, kg.m-2 |
24.3 ± 6.1 |
|
Body Mass Index, kg.m-2
|
<18.5: 26 [14.7] |
|
18.5-24.9: 80 [45.2] |
|
|
≥ 25.0: 71 [40.1] |
|
|
Calf circumference, cm |
30.5 ± 16.9 |
|
Calf circumference, cm
|
<31.0: 98 [55.4] |
|
≥ 31.0: 59 [31.1] |
|
|
Not declared: 20 [11.3] |
|
|
Weight loss, %
|
<5.0 %: 66 [37.3] |
|
5-10 %: 44 [24.9] |
|
|
10-15 %: 36 [20.3] |
|
|
>20 %: 31 [17.5] |
|
|
Serum albumin, g.L-1
|
£ 30: 103 [58.2] |
|
>30: 64 [36.1] |
|
|
Not declared: 10 [ 5.6] |
|
|
C reactive protein, mg.L-1
|
<0.56: 7 [ 3.9] |
|
0.56-4.00: 0 [ 0.0] |
|
|
5.00-50.00: 3 [ 1.7] |
|
|
51.00-100.00: 4 [ 2.3] |
|
|
101.00-200.00: 18 [10.2] |
|
|
>200.00: 32 [18.1] |
|
|
Not declared: 93 [52.5] |
|
|
Source: Records of the study. Size of the serie: 177. |
|
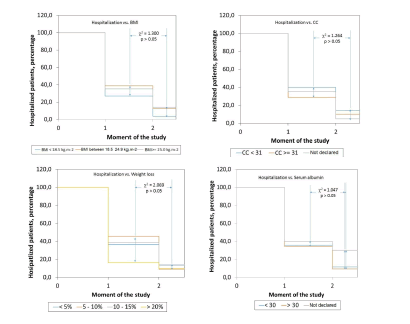
Table 7 shows the associations between the indicators used to describe the nutritional status of GIF patient and outcomes indicators of the study. CC influenced upon prolongation of hospital stay of GIF patients: patients with a diminished CC showed a more prolonged hospital stay: CC<31 cm: 60.3%; CC ≥ 31 cm: 39.0%; CC not annotated/not declared: 26.7% (χ2=12.655; p<0.05; independence test based on the chi-squared distribution) (Table 7). On the other hand, weight loss experienced by the patient exerted a marginal effect upon prolongation of hospital stay (χ2=7.294; p=0.063).
|
Characteristic |
Findings |
Interpretation |
|---|---|---|
|
Survival of the patient |
||
|
Body Mass Index
|
<18.5: 92.3 |
χ2=0.090
|
|
18.5-24.9: 81.3 |
||
|
≥ 25.0: 87.3 |
||
|
Calf circumference
|
<31.0: 86.7 |
χ2=0.623
|
|
≥ 31.0: 84.7 |
||
|
Not declared: 80.0 |
||
|
Weight loss
|
<5.0 %: 81.8 |
χ2=1.128
|
|
5-10 %: 86.4 |
||
|
10-15 %: 88.9 |
||
|
> 20 %: 87.1 |
||
|
Serum albumin, g.L-1
|
£ 30: 85.6 |
χ2=0.246
|
|
>30: 85.9 |
||
|
Not declared: 80.0 |
||
|
Prolonged hospitalization |
||
|
Body Mass Index
|
<18.5: 30.8 |
χ2=3.461
|
|
18.5-24.9: 51.3 |
||
|
≥ 25.0: 49.3 |
||
|
Calf circumference
|
<31.0: 60.3 |
χ2=12.655
|
|
≥ 31.0: 39.0 |
||
|
Not declared: 26.7 |
||
|
Weight loss
|
<5.0 %: 50.0 |
χ2=7.294 |
|
5-10 %: 54.5 |
p = 0.063
|
|
|
10-15 %: 52.8 |
||
|
>20 %: 25.8 |
||
|
Serum albumin, g.L-1
|
£ 30: 47.6 |
c2=2.391
|
|
>30: 43.7 |
||
|
Not declare: 70.0 |
||
|
Spontaneous closure |
||
|
Body Mass Index
|
<18.5: 42.3 |
χ2=0.09
|
|
18.5-24.9: 36.3 |
||
|
≥ 25.0: 33.8 |
||
|
Calf circumference
|
<31.0: 33.0 |
χ2=0.144
|
|
≥ 31.0: 35.6 |
||
|
No declara: 40.0 |
||
|
Weight loss
|
<5.0 %: 30.3 |
χ2=2.174
|
|
5-10 %: 38.6 |
||
|
10-15 %: 44.4 |
||
|
>20 %: 35.5 |
||
|
Serum albumin, g.L-1
|
£ 3.0: 33.0 |
χ2=1.059
|
|
>3.0: 40.6 |
||
|
Not declared: 40.0 |
||
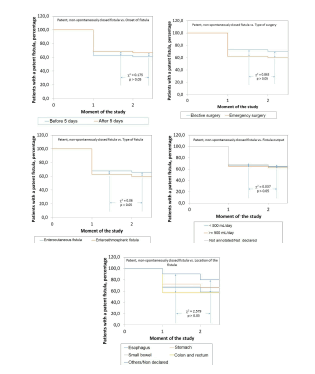
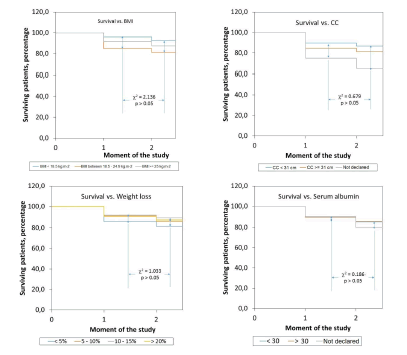
Lastly, Figures 7-9 show the influence of the nutritional indicators upon prognosis and outcomes of GIF. As it can be seen, nutritional status did not influence upon behavior of the study cohort regarding the indicators of prognosis and outcomes of GIF (Figures 7-9).
Figure 9. Behavior of the spontaneous closure of gastrointestinal fistulas in the patients included in the cohort according with their nutritional characteristics as documented on admission in the “Fistula Day” project. Curves were constructed with patients with a patent, non-spontaneously closed fistula, in the corresponding moment of the study.
Discussion
The “Fistula Day” has been conceived as a multi-national, multi-center project aimed to reveal the practices currently followed in the diagnosis and treatment of GIF so, in this way, build the required evidences for the continuous improvement of the quality of surgical and clinical processes. Originally proposed as a Latin-American effort, the “Fistula Day” has also incorporated data provided by medical care teams from hospitals of the United Kingdom and the European Union that requested (and were accepted) to participate in this effort. In spite of this, “Fistula Day” might represent the current state of the treatment of GIF in Latin America, given the fact the majority of the patients being finally included in the database of the project was attended in Latin-American hospitals. It should also be pointed out that more than half of the studied patients were Mexicans: an expected finding giving the preponderance of Mexican health institutions in the database of the study.
The challenge in a research effort of such nature as the one described herein is to integrate all the collected data within a coherent model for interpreting the current reality of the treatment of the GIF. This essay attempted to assess how the characteristics of the patient, on one hand, and those of the fistula per se, on the other; influence upon the prognosis and the outcomes of the GFI through 3 indicators: survival of the patient, prolongation of the hospital stay, and the likely spontaneous closure of the fistula.
Most of the patients included in the “Fistula Day” database were men in their sixth decade of life accumulating between 0-30 days of hospital stay before admission in the present study. A third part of the patients had ages ≥ 60 years: a finding congruent with demographical aging and an increasingly presence of elderlies in the hospital populations. It is to be noticed that cancer was present as primary diagnosis in almost a third of the patients.
After conclusion of the first edition of the “Fistula Day” a 14.7% mortality rate was observed. A systematic review with meta-analysis found a 3.0% average mortality associated with enteral fistulas [12]. Mortality could be as high as 7.0% in patients waiting for a GIF repairing surgery [12]. The authors of the present essay also found a report mentioning 20.0% mortality after repair of entero cutaneous fistulas [13]. On the other hand, Campos et al. reported a 30.9% mortality rate in 188 patients diagnosed and treated with digestive fistulas (with biliopancreatic fistulas amounting for a fifth of them) [14]. Within this context, a 14.7% mortality rate could be perceived as disproportionate, and would lead to further dwell in the causes for it, such as the characteristics of the patient, the fistula, and the hospital admitting and treating him/her, and its organization and the procedures conducted within the institution.
The aforementioned could be also applied to the other two indicators of the prognosis and outcomes of GIF. Hospital stay was prolonged in almost half of the surveyed patients. More than a tenth of the patients initially admitted in the database remained hospitalized after 60 days. Hospital resource is becoming increasingly costly in a setting marked by budgetary and fiscal cuts, along with a greater demand for services and positive impacts. Hence, even a rate>10.0% in the prolongation of hospitalization would imply additional economical burdens thus reducing opportunities for other equally needing patients [15].
Regarding the spontaneous closure of GIF (as the first option for containment and treatment), de Vries et al. have estimated a>80.0% total fistula closure rate reflecting the sums of actions taken in that direction (conservative as well as surgical ones). In the present study, spontaneous closure was achieved only in merely a third of the patients initially admitted in the study. A fistula closure (at least spontaneous) rate<50.0% might point towards failures, insufficiencies and inexperiences in GIF treatment. It is to be noticed Campos et al. reported in their study a 31.4% spontaneous closure rate, when the international literature showed in that particular moment estimates as varied as 23.0% and 80.0% [14].
It could be anticipated the characteristics of the patient might influence in the prognosis and outcomes of GIF, among them subject´s age, previous hospital stay, and cancer diagnosis. Hence, elderlies, patients with prolonged previous hospital stays, and those treated for cancer would distinguish themselves for a lower survival, prolonged hospitalization on closure of the observation window, and a lower rate of spontaneous closure. This was not the case: none of the characteristics of the patient decisively influenced upon the prognosis and outcomes of the fistula.
Similarly, and in correspondence with the accumulated literature, nutritional status of the GIF patient might determine the prognosis and outcomes of the fistula. Fistula is a catastrophic condition for all the domains of the economy, nutritional status in particular, and the resulting malnutrition, in turn, affects survival, prolongs hospital stay, and interferes with the spontaneous closure of the fistula; thus creating a vicious circle hard to break. In the present study, notwithstanding the fact subjects with a BMI ≥ 18.5 kg.m-2 prevailed (suggesting at first a preserved nutritional status), and excessive body weight presented in 40.1% of the cases, more than a third of the patients referred>10% weight loss, half plus one of the patients presented with a diminished CC, and more than half of the GIF patients had a serum albumin<30 g.L-1: these three indicators pointing to an important protein depletion in the study serie. Although protein depletion secondary to GIF could increase the mortality risk of the patient, prolong the hospital stay and/or extend the patency of the fistula, in the present study nutritional status did not influence either upon condition of the patient on the closure of the observation window nor the likelihood of spontaneous closure of the fistula. However, only reduced CC on admission in the study determined a prolonged hospital stay.
Influence of the characteristics of the GIF in its own on the outcomes indicators proposed in this study remains to be considered. It is to be noticed patients with an ECF prevailed, and in most of the instances fistula output was<500 mL/day. It is also to be noticed most of the GIF originated after an emergency surgery. Regarding specialized reports declaring a high frequency of GIF after completion of a bariatric surgery, rate of conduction of these procedures was<4.0% in this study serie [16,17]. Observation of small bowel and colon as the predominant locations of GIF is in line with consulted reports. It was then interesting to see that type of GIF determined subject ´s survival, and (as a complementary phenomenon) the higher mortality observed in this study concentrated among patients with an EAF [12-14]. Exposure of the mucosa has been cited in the specialized literature as one of the factors attempting against the spontaneous closure of the fistula, thus translating to an increased risk of complications (death among them) [18].
Evolution and outcomes of GIF might also be dependent upon location of fistula and the type of surgery associated with this complication, at least, when it comes to prolongation of hospitalization of the patient. Locations of the fistula associated with different rates of prolonged hospitalizations, with fistulas originated in the stomach being associated with the highest rate. However, data paucity (given by the uneven distribution of the cases within the different strata of this category, as it is the case with observational studies) might have obscure this finding. On the other hand, the type of surgery associated with the origin of the fistula might also lead to longer hospitalization, with ECF patients consuming prolonged hospital stays probably because of the conduction of an augmented number of procedures to achieve closure of the fistula.
Conclusion
Evolution and outcomes of GIF might be dependent mainly upon type of the fistula. This association might be “colored” by the location of the fistula and the type of surgery linked with the origin of the fistula, these characteristics determining prolongation of hospital stay. Protein depletion secondary to GIF might also prolong hospital stay of the patient.
Future extensions
Influence of the characteristics of the patient and of the fistula in the evolution and outcomes of GIF has been examined in this essay. However, a comprehensive analysis of this issue would demand the exam of the influence of the characteristics of the hospital. In addition, the methodology of analysis discussed herein would also allow to assess how medical care teams face and deal locally with GIF. These questions will be satisfied in consecutive deliveries.
References
- Pande RK, Gupta A. Gastrointestinal stomas and fistulas: What is lost and what to do. Indian J Crit Care Med 2020;24:S175-8.
[Crossref] [Google scholar] [pubmed]
- Cereatti F, Grassia R, Drago A, Conti CB, Donatelli G. Endoscopic management of gastrointestinal leaks and fistulae: What option do we have?. World J Gastroenterol 2020;26(29):4198-217.
[Crossref] [Google scholar] [pubmed]
- Wheble GA, Knight WR, Khan OA. Enteral vs total parenteral nutrition following major upper gastrointestinal surgery. Int J Surg 2012;10:194-7.
[Crossref] [Google scholar] [pubmed]
- Gronnier C, Chambrier C, Duhamel A, Dervaux B, Collet D, Vaudoyer D, et al. Enteral versus parenteral nutrition in the conservative treatment of upper gastrointestinal fistula after surgery: A multicenter, randomized, parallel-group, open-label, phase III study. Trials 2020;21:448.
[Crossref] [Google scholar] [pubmed]
- Daz-Pizarro Graf JI, Kumpf VJ, de Aguilar-Nascimento JE, Hall AM, McKeever L, Steiger E,et al. ASPEN-FELANPE Clinical Guidelines: Nutrition support of adult patients with enterocutaneous fistula. JPEN J Parenter Enter Nutr 2017;41(1):104-12.
[Crossref] [Google scholar] [pubmed]
- DÂaz-Pizarro Graf JI, Kumpf VJ, de Aguilar-Nascimento JE, Hall AM, McKeever L, Steiger E, et al. Guas Clanicas ASPEN-FELANPE: Terapia nutricional en pacientes adultos con fastulas enterocutaneas. Nutrician Hospitalaria 2020;37(4):875-85.
[Crossref] [Google scholar] [pubmed]
- Marquez HA, Prado RA, Hurtado H, Juarez F, Fernandez J, Mendoza LG, et al. Mexican consensus on the integral management of digestive tract fistulas. Nutrition 1999;15(3):235-8.
[Crossref] [Google scholar] [pubmed]
- Bland JM, Altman DG. The log rank test. BMJ 2004;328:1073.
- Shah PB. Intention-to-treat and per-protocol analysis. CMAJ 2011;183(6):696.
[Crossref] [Google scholar] [pubmed]
- Berger ML, Sox H, Willke RJ, Brixner DL, Eichler HG, Goettsch W, et al. Good practices for real world data studies of treatment and/or comparative effectiveness: Recommendations from the joint ISPORAISPE Special Task Force on real world evidence in health care decision making. Pharmacoepidemiol Drug Saf 2017;26(9):1033-9.
[Crossref] [Google scholar] [pubmed]
- World Medical Association. Declaration of Helsinki on the ethical principles for medical research involving human subjects. Assist Inferm Ric 2001;20(2):104-7.
- de Vries FEE, Atema JJ, van Ruler O, Vaizey CJ, Serlie MJ, Boermeester MA. A systematic review and meta-analysis of timing and outcome of intestinal failure surgery in patients with enteric fistula. World J Surg 2018;42:695-706.
[Crossref] [Google scholar] [pubmed]
- Martinez JL, Luque de Len E, Ballinas Oseguera G, Mendez JD, Juarez Oropeza MA, Roman Ramos R. Factors predictive of recurrence and mortality after surgical repair of enterocutaneous fistula. J Gastrointest Surg 2012;16:156-63.
[Crossref] [Google scholar] [pubmed]
- Campos ACL, Andrade DF, Campos GMR, Matias JEF, Coelho JCU. A multivariate model to determine prognostic factors in gastrointestinal fistulas. J Am Coll Surg 1999;188:483-90.
[Crossref] [Google scholar] [pubmed]
- Clements B, Coady D, Gupta S. The economics of public health care reform in advanced and emerging economies. International Monetary Fund. Washington DC: 2012. Chapter 1. Pp 6.
- Santo MA, Pajecki D, Riccioppo D, Cleva R, Kawamoto F, Cecconello I. Early complications in bariatric surgery. Arq Gastroenterol 2013;50:50-5.
[Crossref] [Google scholar] [pubmed]
- Bhayani NH, Swanstram LL. Endoscopic therapies for leaks and fistulas after bariatric surgery. Surgical Innovation 2014;21:90-7.
[Crossref] [Google scholar] [pubmed]
- Giudicelli G, Rossetti A, Scarpa C, Buchs NC, Hompes R, Guy RJ,et al. Prognostic factors for enteroatmospheric fistula in open abdomen treated with negative pressure wound therapy: A multicentre experience. J Gastrointest Surg 2017;21:1328-34.
[Crossref] [Google scholar] [pubmed]
Copyright: © 2022 The Authors. This is an open access article under the terms of the Creative Commons Attribution-NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.