Original Article - Archives of Clinical and Experimental Surgery (2025)
The Physics of Intussusception Reduction
Ramendra Shukla1*, Sudhir B Chandna1 and Rasna Tiwari22Department of Nuclear Medicine, HCG Hospital, Ahmedabad, Gujarat, India
Ramendra Shukla, Department of Paediatric Surgery, Smt NHL Medical College and SVP Institute of Medical Sciences and Research,Ahmedabad, Gujarat, India, Email: drramendrashukla@gmail.com
Received: 28-Jul-2025, Manuscript No. EJMACES-25-170828; Editor assigned: 31-Jul-2025, Pre QC No. EJMACES-25-170828 (PQ); Reviewed: 14-Aug-2025, QC No. EJMACES-25-170828; Revised: 28-Aug-2025, Manuscript No. EJMACES-25-170828 (R); Published: 26-Sep-2025
Abstract
Aim: To understand the scientific basis of intussusception reduction and to determine the effectiveness and success rate of pneumatic reduction and also to identify factors that predict an unsuccessful outcome.
Materials and Methods: This retrospective study was carried out in 50 patients of intussusception aged 2 months to 11 years from January 2020 to December 2024. Pneumatic reduction of intussusception was carried out in the standard manner, when a pressure of approximately 100 mm of Hg was applied. Applying Pascal’s principle and Laplace’s law, the pressure could be raised to 120 mm of Hg if the lower pressure was not working. Presenting signs and symptoms, results of radiological investigations, the outcome of attempted reduction, complications and any subsequent surgical interventions were examined.
Results: Successful pneumatic reduction was achieved in 33 (66%) cases during the study period. The mean age at presentation was 1 year (range: 2 months to 12 years). The only significant predictor of failure was long duration of symptoms (p<0.05). Among the 17 cases of failed reduction, surgery was performed and the findings were colo-colic intussusception (n=2), ileo-ileo-colic intussusception (n=1) and ileocolic intussusception (n=14). Resection anasmotosis (n=8), manual reduction+ appendicectomy (n=7) and Meckel’s Diverticulectomy (n=2) was done. No deaths occurred during the study period.
Conclusion: Fluoroscopy-guided pneumatic reduction of intussusception offers a high success rate (66%) without any complications. As the gas molecules are loosely packed, it is possible to apply a little higher pressure (120 mm of Hg) vis-a-vis liquids, which have densely packed molecules. The most important predictor of outcome in this study was the long duration of symptoms.
Introduction
Intussusception is the most common cause of bowel obstruction in infants and toddlers and can result in considerable morbidity and mortality if not promptly treated [1]. It can be managed by both surgical and non-surgical methods. Nonsurgical methods include ultrasound and fluoroscopy-guided hydrostatic and pneumatic reduction. All these methods have been tried and accepted in many countries. Many studies suggest that fluoroscopy-guided pneumatic reduction is superior to liquid enema for various reasons. It is easier to perform, it is less messy, there is less radiation dose and if perforation does occur, there is less soiling of the peritoneal cavity.
In this study, we have tried to unravel the physics behind the reduction procedure and present our experience with 50 cases managed during a period of five years.
The first-line treatment of choice in uncomplicated cases of intussusception at our institution remains fluoroscopically guided pneumatic reduction. The aim of this study was also to determine the success rate of pneumatic reduction of intussusception in a tertiary-level institute and to identify the factors that could predict an unsuccessful outcome.
Materials and Methods
This is a 5-year retrospective study conducted between January 2020 and December 2024. There were 50 cases with the age ranging from 2 months to 11 years. There were 28 males and 22 females and the duration of symptoms ranged from a few hours to 4 days. As none of the patients presented with perforation and/or signs of peritonitis, they were first subjected to pneumatic reduction under fluoroscopic control. The pressure was kept at around 100 mm of Hg.
Statistical analysis was performed using Chi-square test and degree of freedom was kept as 1 and for that table value is 3.84.
If calculated value was more than 3.84, then the p<0.05.so that the difference becomes significant.
Five variables were analyzed as potential predictors of outcome:
• Age
• Gender
• Duration of symptoms
• Bleeding per rectum
• Palpable abdominal mass
The level of statistical significance was set at 5%.
Results
Pneumatic reduction was successful in 66% of cases (33 of 50 cases). Of the 33 successes, 15 were reduced by single insufflation, 16 were reduced by 2 insufflations and 2 by 3 insufflations. The mean age of presentation was 1 year (range: 2 months to 12 years). In children under the age of 12 months, reduction was successful in 68% (17/25 patients), while in those over 1-year-old, it was successful in 64% (16/25 patients) (Table 1).
| Clinical features | Frequency | Percentage |
|---|---|---|
| Abdominal pain | 44 | 88% |
| Vomiting | 37 | 74% |
| Red Currant Jelly stool | 36 | 72% |
| Lump in abdomen | 20 | 40% |
| Fever | 19 | 38% |
| Diarrhoea | 18 | 36% |
| Lethargy | 13 | 26% |
| Abdominal distention | 10 | 20% |
Table 1. Displays various symptoms in decreasing order of percentage.
The duration of symptoms varied with a mean duration of 2 days prior to presentation; 68.42% of patients (13/19) who had been symptomatic for ≥ 2 days failed pneumatic reduction, whereas only 12.90% of patients (4/31) who presented <2 days after becoming ill had failed reduction (p<0.05). This was statistically significant.
Rectal bleeding was present in 36 cases
The success rate of pneumatic reduction was 69.44% (25/36) for patients with rectal bleeding and 57.14% (8/14) for those without haematochezia (p>0.05.).
A palpable abdominal mass was documented as present in 64% (32/50) of the patients, but no significant difference (p>0.05) was found between these groups vis-a-vis success achieved with pneumatic reduction.
Out of total 50 cases of intussusception, obstruction was relieved in 33 patients by pneumatic reduction whereas 17 patients required operative management.
Surgical procedure
There was no incidence of bowel perforation during pneumatic reduction. In patients where pneumatic reduction was successful, there was no recurrence of signs and symptoms of intussusception during the 24-hour observation before discharge. These patients were well at two weeks of follow-up (Table 2).
| Surgical procedure | Frequency(n=17) | Percentage |
|---|---|---|
| Resection anastomosis | 8 | 47.05% |
| Manual reduction+Appendicectomy | 7 | 41.18% |
| Meckel’s diverticulectomy | 2 | 11.77% |
Table 2. Suggesting various operative procedures in decreasing percentage apart from pneumatic reduction.
Above 17 specimens were sent for histopathological report and the following are there diagnosis (Table 3).
| Histopathological diagnosis | Frequency (n=17) | Percentage |
|---|---|---|
| Appendicitis (Acute/Chronic) | 11 | 64.70% |
| Gangrenous changes in intussuscepted bowel segment | 4 | 23.52% |
| Inflammation of Meckel’s diverticulum | 2 | 11.76% |
| Non-Hodgkin’s lymphoma | 1 | 5.88% |
Table 3. Various histopathological diagnoses we came across after surgical procedures.
Out of the above 17 patients, one patient had gangrenous changes in the intussuscepted ileum along with acute appendicitis.
Discussion
Intussusception is one of the most common cause of abdominal pain and intestinal obstruction in infants [1]. Less than 10% of patients have a pathological lead point with 2:1 male preponderance [2].
In our series, there was a slight male preponderance, with 5% of the patients having a lead point as discovered at surgery.
The reported success rate of pneumatic reduction has ranged from 27% to 96% and many authors have reported it to be more than 90% [3-4].
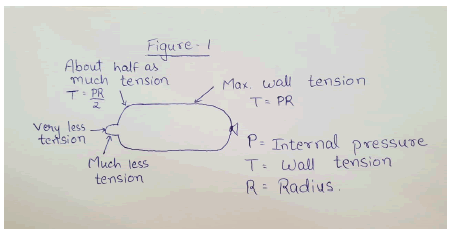
We delved into the physics of this process of reduction. According to Pascal’s principle, the pressure is same inside a balloon that is inflated and the end is tied. But if one end of this balloon is dipped in liquid nitrogen to contract it, then there are great differences in wall tension on different parts of the balloon (Figure 1).
Figure 1. Showing the role of Pascal’s principle in a balloon when one end is tied and the other constricted.
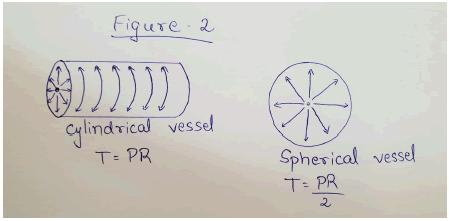
This variation is described by Laplace’s law. According to Laplace’s law, the larger the vessel radius, the larger the wall tension required to withstand a given internal fluid pressure. (Figure 2).
Figure 2. Demonstrating the tension developing based on the internal radius of a vessel. Tension is directly proportional to the internal radius of a vessel.
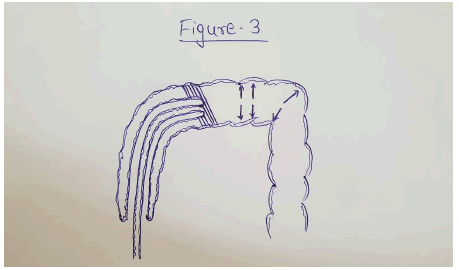
Applying this to intussusception, there is relatively less wall tension required to withstand the pressure where the apex of the intussusceptum is, as the radius is less (the striped areas). So the perforation, if it takes place, will take place in the intestine distal to this point, where the radius is much more (Figure 3).
Figure 3. Showing the effect of Laplace’s law in causing perforation and its site in the intussuscepted segment of bowel.
As regards to hydrostatic vs. pneumatic reduction, in a fluid at rest in a closed container, a pressure change in one part is transmitted without loss to every position of the fluid and to the wall of the container. A liquid like water is only very slightly compressible because there is not much space between the molecules, so pressure change is uniform throughout. This perhaps explains the slightly better rate of reduction achieved with liquid enema in some centres [5].
In the case of gas, there are big spaces between the molecules and the Pascal’s law does not apply as generally as it does for nearly incompressible liquids, so the value of P is somewhat less than the applied pressure. Keeping this in mind, during the latter half of our study, if there was no reduction using air with a pressure of 100 mm of Hg, we went up to 120 mm of Hg.
Our overall success rate of pneumatic reduction was 66% with a slight gradual improvement in the later years of the study. There was no perforation in our series. This is in accordance with other reported cases of <1% [6-8].
If perforation does occur, tension pneumoperitoneum can cause a fatal outcome and should be promptly relieved with an 18-gauge needle before proceeding to surgery.
Of the five variables studied in this series, the most significant predictor of the success of reduction was the duration of the symptoms.
Conclusion
By understanding the principle of physics guiding the reduction of intussusception, we can conclude that:
- The pressure applied via liquid enema is unchanged at the point where it acts on the intussusceptum.
- In the case of air, there is some loss of this pressure as the molecules are loosely packed, so a pressure of 120 mm of Hg can be applied if a lesser pressure is not achieving the reduction.
- The perforation, if it occurs, will be at a point where the radius of the colon is maximum, as the wall tension required to withstand the pressure will be much greater.
- The only statistically significant variable affecting the outcome of reduction was the duration of the symptoms.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given their consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal patient identity, but anonymity cannot be guaranteed.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- Jay J, O’Neill A. Pediatric surgery. Grosfeld James 2015;85:1090-1110.
- Mark M, Ravitch. Pediatric surgery. 2013;88:850-861.
- Meyer JS, Dangman BC, Buonomo C, Berlin JA. Air and liquid contrast agents in the management of intussusception: A controlled, randomized trial. Radiology 1993;188(2):507-511.
[Crossref] [Google Scholar] [PubMed]
- Kirks DR. Air intussusception reduction: "The winds of change". Pediatr Radiol 1995;25(2):89-91.
[Crossref] [Google Scholar] [PubMed]
- Khorana J, Singhavejsakul J, Ukarapol N. Enema reduction of intussusception: the success rate of hydrostatic and pneumatic reduction. Ther Clin Risk Manag 2015:1837-1842.
[Crossref] [Google Scholar] [PubMed]
- Davenport M, Spitz L, Coran A, editors. Operative pediatric surgery. CRC Press. 2013.
- Moritz M. Ziegler, Thomas R. Operative pediatric surgery. Weber 57:645- 660
- Ashcraft’s paediatric surgery. 5th edition. 39:500-539.
Copyright: © 2025 The Authors. This is an open access article under the terms of the Creative Commons Attribution Non Commercial Share Alike 4.0 (https:// creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.