Research - Archives of Clinical and Experimental Surgery (2023)
Utility of Bipaddle Pectoralis Major Myocutaneous Flap Reconstruction for Single Stage Reconstruction in Locally Advanced Oral Cancer
Bhavesh Bang, Hemant Thanna* and Manish KaushalHemant Thanna, Department of General Surgery, MGM Medical College, Indore, India, Email: thannaailash@gmail.com
Received: 15-Jul-2023, Manuscript No. EJMACES-23-106464; Editor assigned: 18-Aug-2023, Pre QC No. EJMACES-23-106464 (PQ); Reviewed: 02-Aug-2023, QC No. EJMACES-23-106464; Revised: 09-Aug-2023, Manuscript No. EJMACES-23-106464 (R); Published: 16-Aug-2023
Abstract
Back ground: India has the unfortunate distinction of being the oral cancer capital of the world. Most oral cancers in India present in the advanced stages of their disease (TNM stage III and IV) (Tumor (T), Node (N), and Metastasis (M) staging), as compared to the West, where the majority of patients present in stage I and II. Advanced oral cancer poses challenges not only with respect to resection but also in terms of reconstruction. While microvascular free tissue transfer is the standard of care now at most western centres, the Pectoralis Major Myo Cutaneous (PMMC) flap still forms the workhorse for oral cavity reconstruction following ablative surgery for cancer at most centres in India. For through-and-through defects of the oral cavity, the approach has been to perform the PMMC flap for the mucosal lining and a second fasciocutaneous flap for the outer cover. This, however, makes the surgery a two-stage procedure, increasing the morbidity.
Method: We present our series of 20 patients with locally advanced oral cancer treated by surgery, resulting in full-thickness defects of the oral cavity, who were reconstructed using a bipaddle PMMC flap, offering a single-stage reconstruction of the defect. This was a prospective observational study, conducted over one year.
Conclusion: Our study upholds the utility of doing a bipaddle PMMC flap in advanced oral carcinoma as previously reported in the literature.
Keywords
Oral cancer; PMMC flap; Bipaddle; Surgery
Introduction
Oral squamous cell cancer is one of the most common cancers in India. Surgery is the primary treatment modality for the majority of oral cancers. Most patients with oral cancer in India present in advanced stages of the disease, where surgery results in full-thickness defects of the oral cavity. While free tissue transfer is considered the standard of care for the reconstruction of Head and Neck cancer defects, the use of this technique is still not common at many centres in India owing to the restrictions of expertise and resources. Pectoralis Major Myo Cutaneous (PMMC) flap has earned the title of “workhorse flap” in Head and Neck reconstruction. Large defects arising from the excision of oral cancer involving mucosa as well as the skin were traditionally reconstructed using a PMMC flap for the mucosa and another fasciocutaneous flap like a deltopectoral or a forehead flap for the outer skin cover. This, however, converted the reconstructive surgery into a two-stage process requiring the division of the fasciocutaneous flap after 3 weeks and also needed additional procedures like skin grafting over the fasciocutaneous flap donor site. The use of bipaddle, folded PMMC flaps has brought a paradigm shift in the reconstruction of large oral defects. This technique is also useful in salvage situations following necrosis of free flaps.
Ariyan in 1979 introduced the PMMC flap into head and neck reconstruction [1]. Pectoralis Major Myo Cutaneous (PMMC) flap has the advantage of being in proximity to the head and neck region [2] . The main goal of reconstruction is to provide intraoral lining and soft tissue cover. Bipaddle Pectoralis Major Myocutaneous flap is a modification of the PMMC flap which utilizes two skin islands for reconstruction of composite oral defects. The first use of PMMC as a bipaddle flap was also reported by Ariyan in 1979 [3]. The use of this technique had diminished with the arrival of free flaps. However, the technique is still relevant in the Indian context, where infrastructure and skills for performing microvascular-free flaps may not be available. This technique also finds usefulness as a salvage method of reconstruction following free flap failure [4,5].
Materials and Methods
Study design
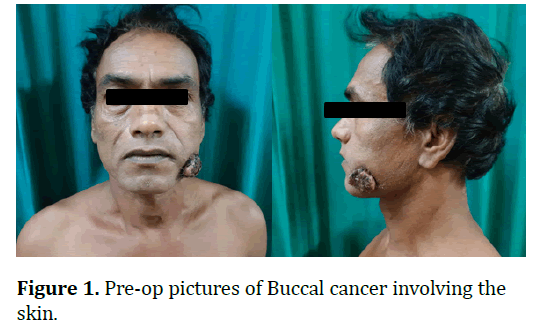
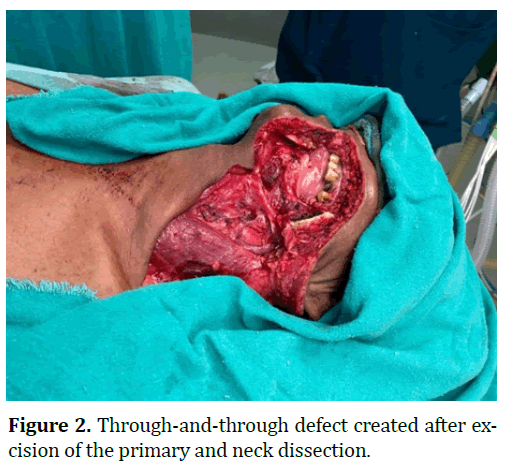
An observational study was done from November 2020 to November 2021 on 20 patients of clinical T4a Oral cancer of Squamous Cell Carcinoma (SCC) who underwent wide local excision of the primary tumour along with comprehensive or selective neck dissection with reconstruction done using the Bipaddle PMMC flap. All patients had either a gross involvement of the skin with fungating tumour or the tumour was close to the skin, and R0 resection was not possible without skin resection. The study was approved by the institutional review board and ethics committee.
Surgical technique
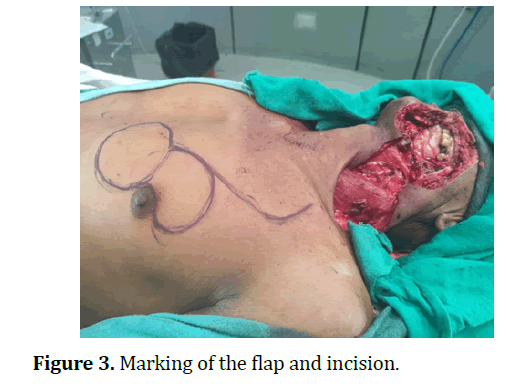
The patient lies in a supine position with an extended neck and turned to the opposite side. The clavicle, xiphoid, and ipsilateral sternal border are identified and marked. The size and location of the skin paddle are marked on the inferior-medial border of the pectoralis major muscle. The vascular axis is drawn on the skin of the chest.
The initial incision is made at the lateral part toward the anterior axillary line down to the pectoralis major muscle. The maximum amount of muscle should be harvested, because the larger the muscle volume, the safer the flap due to the increased number of myocutaneous perforators.
The inferior, medial and lateral incisions are made through the skin, subcutaneous fat and pectoralis fascia down to the chest wall. The superior incision is made down to the muscle fibres and the skin island is tightened to the muscle with absorbable sutures to protect the shearing effect on the skin island during operative handling. As the muscle is elevated inferiorly to superiorly, the pedicle should be identified by visualization on the undersurface of the muscle. Shining a light through the muscle aids in the visualization of the pedicle. The pectoralis major muscle derives its blood supply from the pectoral branch of the thoracoacromial artery and lateral thoracic artery. During the dissection, the vascular bundle should always be seen in order to avoid injury to this bundle. After the dissection of the flap, a subcutaneous tunnel is formed under the skin between the neck (preserving the perforators to the overlying deltopectoral flap) and the chest and the flap is passed underneath the skin bridge.
Sternomastoid muscle was removed to accommodate the pedicle of the PMMC flap into the neck for the initial 6 patients. Later, we found this to be unnecessary and modified the surgical technique to preserve the steroncological nomostoid muscle in situ, which was removed only for steroncological indications. Care was taken to preserve the perforators of the deltopectoral flap while marking the skin incision for the PMMC flap.
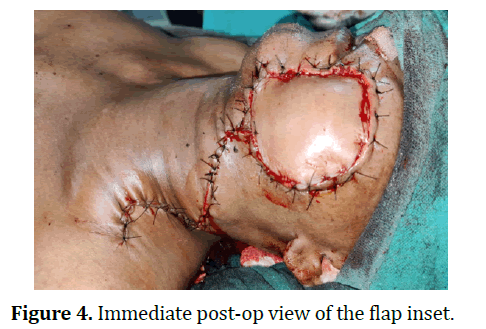
Our preferred method of flap orientation was transverse. In most cases with large defects, the inferolateral edge of the flap lies outside the territory of the muscle for a varying distance of 2-5 cm. Since supply to the skin comes from musculocutaneous perforators this territory has a random patterned blood supply, making it more susceptible to necrosis. This lateral portion of the flap was preferentially placed on the inside, as the necrosis and flap dehiscence of this region is easier to manage.
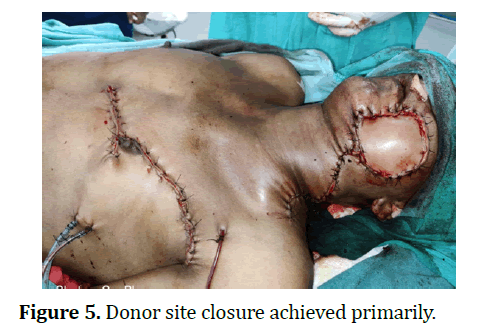
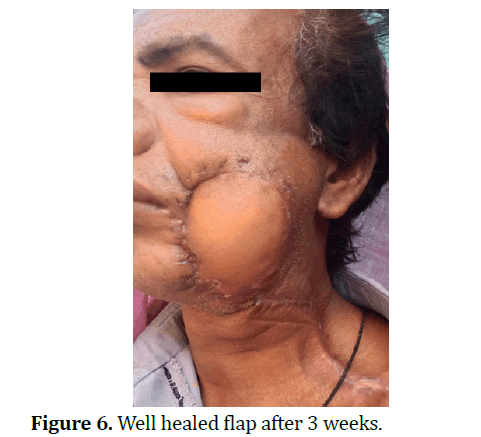
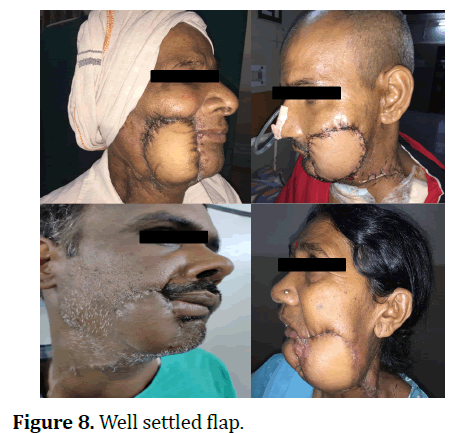
The intervening portion of the flap between two skin paddles was de-epithelized to allow for the folding of the flap. Flap was inset in the usual fashion. If the oral commissure was involved, we preferred to do inset in a manner which would keep the oral competence intact, even if it caused some amount of microstomia. The donor site was closed after placing the negative suction drains. In spite of the large flap size, primary closure of the donor site was achieved in all 20 cases (Figures 1-8).
Results
The patient, tumor and surgical details are listed in Table 1.
| Variable | N (%) | |
|---|---|---|
| Gender | Male | 15 (75%) |
| Female | 5 (25%) | |
| Age group | 30-40 years | 3 (15%) |
| 40-50 years | 7 (35%) | |
| 50-60 years | 7 (35%) | |
| >60 years | 3 (15%) | |
| Side of lesion | Right | 14 (70%) |
| left | 6 (30%) | |
| Comorbidity | Diabetes | 3 (15%) |
| Hypertension | 4 (20%) | |
| Diabetes and Hypertension | 1 (5%) | |
| No comorbidity | 12 (60%) | |
| Primary tumor site | Buccal mucosa | 8 (40%) |
| Lower alveolus | 4 (20%) | |
| Lower GB sulcus | 2 (10%) | |
| Retromolar area | 6 (30%) | |
| Oral commissure involved | Yes | 14 (70%) |
| No | 6 (30%) | |
| Flap area | Maximum | 98 cm2 |
| Minimum | 40 cm2 | |
| Average | 58 cm2 | |
| Surgical time | Maximum | 183 |
| Minimum | 289 | |
| Average | 224 |
Table 1. Patient and tumor characteristics.
Out of 20 patients, 15 (75%) were male and 5 females (25%). Age ranged from 32 years to 67 years with peak incidence in patients between 40-60 years of age accounting for 70%. The tumor was on the left side in 30 % and 70% on the right side of the oral cavity.
The most common primary tumor site was buccal mucosa (40%), followed by retromolar trigone (30%). The defects of skin and mucosa were measured separately before flap harvesting and flap marking was done accordingly over the donor site, with two separate paddles marked before harvesting. The maximum size of mucosal defect was 7 cm × 5 cm while the largest skin defect was 10 cm × 8 cm. The largest flap was 14 cm ×7 cm in size (98 cm2 ), while the smallest flap was 8 cm × 5 cm (40 cm2 ). The average flap size was 58 cm2 .
The average surgical time (time of incision to last suture) in our study was 224 mins. We followed a single-team approach in which reconstruction was followed by resection. The average postoperative hospital stay was 14 days.
Complications are listed in Table 2. Complications were noted mostly at the recipient site. There was no complete flap loss in the study.
| Complication | N (%) |
|---|---|
| Orocutaneous fistula | 4 (20%) |
| Donor site seroma | 2 (10%) |
| Partial flap necrosis | 6 (30%) |
| Donor site infection | 2 (10%) |
| Recipient site infection | 6 (30%) |
| Drooling of saliva | 8 (40%) |
| Adjuvant treatment delay | 4 (20%) |
Table 2. Complications.
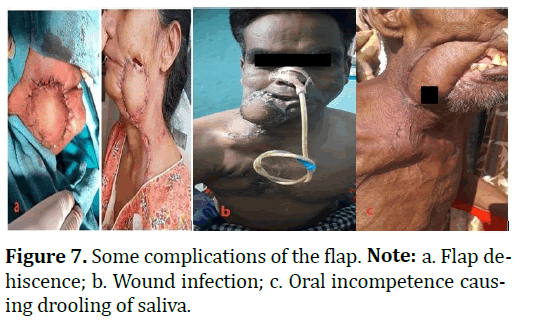
Two patients (10%) had seroma at the flap donor site, which was managed conservatively with repeated aspirations. Four patients (20%) developed an orocutaneous fistula because of flap dehiscence. Six (30%) patients had partial flap necrosis, which was managed conservatively by debridement and re-suturing. Six patients (30%) had an infection at the recipient site while 2 (10%) had donor site infection. All the infections were minor and managed conservatively by stepping up the antibiotics. In spite of our policy of giving priority to keeping oral competence intact, at the cost of microstomia, most patients with commissure involve involvement (n=14, 70%) developed oral incompetence (n=8, 40%).
Four patients (20%) faced a delay in the initiation of adjuvant treatment because of post-operative complications.
Discussion
Pectoralis Major Myo Cutaneous flap (PMMC) has been employed as a reliable choice for the reconstruction of the defect after resection of cancer of the oral cavity. Because of its reliable vascularity and ease of harvesting, PMMC flap is still the most popular flap, especially in developing countries [6-8]. The flap can be used in both primary as well as salvage settings. The main advantage of PMMC flap which makes it popular amongst surgeons treating oral cancer is a short learning curve [9]. Since its introduction in 1979, the harvesting technique of the flap has remained constant, with very few modifications. Use of this flap as a bi-paddle flap became popular in developing countries with a high burden of oral cancer because of a need to provide both inner and outer lining for through-and-through defects of the oral cavity. In India, majority of oral cancers present in an advanced stage of the disease, making this technique particularly useful for single stage reconstruction.
In this study, all patients had oral squamous cell carcinoma, requiring a composite resection resulting in a full thickness, through-and-through defect of the oral cavity.
Published data for age and sex distribution of oral cancers is in accordance with our study. Previous studies have shown similar age and sex distribution of oral cancers found in our study [10,11].
The reliability and safety of bi-paddle PMMC has been shown by various authors in the past. Flap success rates of over 90% have been reported in various studies. Back in 1982, Weaver, et al [12] described the use of “bilobular” flap in eight patients with no incidence of flap necrosis. Similar results have been reported in later studies by Bhathena, et al [4] and Ahmed, et al [13]. Complications, though minor in most cases are frequent following a PMMC flap. The Main complications noted in our study were wound infection, drooling of saliva, and wound dehiscence.
Konduru, et al [14] in their study of 41 bi-paddle PMMC flaps showed a complication rate similar to the conventional PMMC flap. Partial necrosis of the flap, flap dehiscence, oral incompetence and oro-cutaneous fistula are some of the common complications reported in the literature. Shah et al [15] in their large retrospective series of 211 patients reported that only 22% of patients had an uneventful recovery, while 63% of patients developed flap related complications and 14% developed complications not related to the flap. Many flap related complications are interlinked and it is not uncommon to see multiple complications in a single patient. For example, a patient developing flap dehiscence is more prone to have subsequent wound infection and risk of oro-cutaneous fistula formation. In large PMMC flaps, like bipaddle flaps, a large portion of skin is not above the muscle and the blood supply to such regions is in random pattern from the nearby skin. This increases the possibility of partial flap necrosis immensely and it has been reported to be one of the main complications in various studies.
Though it is one of the most popular flaps in use today, even after the arrival of free flaps, there are several potential disadvantages of PMMC flap [2,16,17]. The thick layer of subcutaneous fat and breast tissue can make the flap too bulky, especially in female patients and when used as a bi-paddle flap. Deformity of breasts is another area of concern in female patients. In male patients, excessive intra-oral growth of hair may be troublesome for some patients. The flap has a limited reach and cannot be used for defects above the zygomatic arch, making it less suitable for use in patients who undergo infratemporal fossa clearance, which is increasingly been performed for oral cancer. While the skin of the flap provides a supple surface for mucosalisation, the pectoralis major muscle often atrophies and creates a contracture in the neck, which impairs neck mobility.
Conclusion
Bipaddle Pectoralis Major Myocutaneous flap has been used successfully in patients for reconstruction of mucosal and skin defect after resection of oral cancer. This flap provides a large bulk of vascularized muscle and skin paddle of appropriate size to cover the defect. Bipaddling of flap has advantage that mucosal and skin defect can be filled by single flap. The Pectoralis major flap is easy to harvest as its vascular pedicle i.e., pectoral branch of thoracoacromial artery can be easily identified. The main complications were partial flap necrosis, flap dehiscence and drooling of saliva. Majority of complications were managed conservatively, only a few patients required minor operative intervention. To conclude our study the bipaddle PMMC Flap is a reliable option for reconstruction in oral cancer patient with less postoperative complications and good cosmetic outcome.
References
- Ariyan S. The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg 1979;63(1):73-81.
[Crossref] [Google Scholar] [Pubmed]
- Milenović A, Virag M, Uglešić V, Aljinović-Ratković N. The pectoralis major flap in head and neck reconstruction: First 500 patients. J Craniomaxillofac Surg 2006;34(6):340-343.
[Crossref] [Google Scholar] [Pubmed]
- Ariyn S. Further experiences with the pecoris major myocutaneous flap for the immediate repair of defects from excisions of head and neck cancer. Plast Reconstr Surg 1979;64:605-612.
[Google Scholar] [Pubmed]
- Bhathena HM, Kavarana NM. The folded, bipaddled pectoralis major composite flap in oral cancer reconstruction. Br J Plast Surg 1989;42(4):441-446.
[Crossref] [Google Scholar] [Pubmed]
- Liu M, Liu W, Yang X, Guo H, Peng H. Pectoralis major myocutaneous flap for head and neck defects in the era of free flaps: Harvesting technique and indications. Sci Rep 2017;7(1):46256.
[Crossref] [Google Scholar] [Pubmed]
- Kruse AL, Luebbers HT, Obwegeser JA, Bredell M, Grätz KW. Evaluation of the pectoralis major flap for reconstructive head and neck surgery. Head Neck Oncol 2011;3:1-6.
[Crossref] [Google Scholar] [Pubmed]
- Bhola N, Jadhav A, Borle R, Khemka G, Kumar S, Shrivastava H, et al. Is there still a role for bilobed/bipaddled pectoralis major myocutaneous flap for single-stage immediate reconstruction of post ablative oncologic full-thickness defects of the cheek?. Oral Maxillofac Surg 2015;19:125-131.
[Crossref] [Google Scholar] [Pubmed]
- Gadre KS, Gadre P, Sane VD, Halli R, Doshi P, Modi S, et al. Pectoralis major myocutaneous flap—Still a workhorse for maxillofacial reconstruction in developing countries. J Oral Maxillofac Surg 2013;71(11): e1-2005.
[Crossref] [Google Scholar] [Pubmed]
- McLean JN, Carlson GW, Losken A. The pectoralis major myocutaneous flap revisited: A reliable technique for head and neck reconstruction. Ann Plast Surg 2010;64(5):570-573.
[Crossref] [Google Scholar] [Pubmed]
- Vural E, Suen JY. The submental island flap in head and neck reconstruction. Head Neck 2000;22(6):572-578.
[Crossref] [Google Scholar] [Pubmed]
- Chen WL, Li J, Yang Z, Huang Z, Wang J, Zhang B. Extended vertical lower trapezius island myocutaneous flap in reconstruction of oral and maxillofacial defects after salvage surgery for recurrent oral carcinoma. J Oral Maxillofac Surg 2007;65(2):205-211.
[Crossref] [Google Scholar] [Pubmed]
- Weaver AW, Vandenberg Jr HJ, Atkinson DP, Wallace JR. Modified bilobular (“gemini”) pectoralis major myocutaneous flap. Am J Surg 1982;144(4):482-488.
[Crossref] [Google Scholar] [Pubmed]
- Ahmad QG, Navadgi S, Agarwal R, Kanhere H, Shetty KP, Prasad R, et al. Bipaddle pectoralis major myocutaneous flap in reconstructing full thickness defects of cheek: A review of 47 cases. J Plast Reconstr Aesthet Surg 2006;59(2):166-173.
[Crossref] [Google Scholar] [Pubmed]
- Konduru V, Tirkey AJ, Samy K, Devarakonda KK, Janakiraman R. The folded, bipaddled pectoralis major myocutaneous flap for complex oral cavity defects: Undiminished relevance in the era of free flaps. JPRAS Open 2021;27:108-118.
[Crossref] [Google Scholar] [Pubmed]
- Shah JP, Haribhakti V, Loree TR, Sutaria P. Complications of the pectoralis major myocutaneous flap in head and neck reconstruction. Am J Surg 1990;160(4):352-355.
[Crossref] [Google Scholar] [Pubmed]
- Vartanian JG, Carvalho AL, Carvalho SM, Mizobe L, Magrin J, Kowalski LP, et al. Pectoralis major and other myofascial/myocutaneous flaps in head and neck cancer reconstruction: Experience with 437 cases at a single institution. Head Neck 2004;26(12):1018-1023.
[Crossref] [Google Scholar] [Pubmed]
- Metgudmath RB, Metgudmath AR, Metgudmath VV, Roy B, Das AT. Versatility of pectoralis major myocutaneous flap in oncosurgery and its role in developing countries. Indian J Otolaryngol Head Neck Surg 2013;65:80-84.
[Crossref] [Google Scholar] [Pubmed]
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution NonCommercial ShareAlike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.