Research Article - Archives of Clinical and Experimental Surgery (2023)
Outcomes of Laparoscopic TAPP Inguinal Hernia Repair without Mesh Fixation
Sajid Iqbal1* and Saima Tabassum22Department of Health, Maharishi Markandeshwar Institute of Medical Sciences and Research, Haryana, India
Sajid Iqbal, Department of Surgery, Maharishi Markandeshwar Institute of Medical Sciences and Research, Haryana, India, Email: drsajid.iqbal@gmail.com
Received: 27-Jan-2023, Manuscript No. EJMACES-23-86997; Editor assigned: 30-Jan-2023, Pre QC No. EJMACES-23-86997 (PQ); Reviewed: 16-Feb-2023, QC No. EJMACES-23-86997; Revised: 23-Feb-2023, Manuscript No. EJMACES-23-86997 (R); Published: 03-Mar-2023
Abstract
Inguinal hernia repair is one of the commonest general surgical procedures performed worldwide. Laparoscopic repair is associated with faster recovery, less post-operative pain and comparable rates of recurrence. Using the stapling devices increases post Trans Abdominal Pre Peritoneal (TAPP) chronic groin pain. We conducted a prospective trial for laparoscopic TAPP inguinal hernia repair on 43 patients in which we did not fix the mesh. The primary purpose of this study was to examine the rate of recurrence and chronic groin pain in patients undergoing TAPP mesh hernia repair for inguinal hernia. We observed that our rates of recurrence and chronic groin pain are comparable to those described previously in the literature. We concluded that laparoscopic inguinal hernia repair by TAPP approach can be done with acceptable rates of recurrences and decreased rates of post-operative chronic groin pain
Keywords
Inguinal hernia; TAPP; laparoscopy; Mesh
Introduction
Aims and objectives of the paper is to study the outcome of laparoscopic Trans Abdominal Pre Peritoneal (TAPP) without mesh fixation. Conservative management of inguinal hernia was first reported by Egyptian physicians 300 years ago. Tissue repair by Bassini remained widely practiced till Lichtenstein quoted tension free mesh repair offering lesser recurrence rates, approx 5% vs. 15%. Open mesh repair procedures are plagued by chronic groin pain in 53% patients. Laparoscopic approach offers comparable results with reduced rate of chronic groin pain, <1% [1]. While many surgeons performing laparoscopic Totally Extra Peritoneal (TEP) repair do not routinely use mesh fixation devices. At present, there is still a tendency to fix the mesh with staples or tacks during TAPP to avoid hernia recurrence. Studies relate the chronic groin pain to staples and tacks used while fixing the mesh to the cooper ligament and anterior abdominal wall. Avoiding the use of a mesh fixation device is therefore likely to reduce the rates of chronic groin pain after TAPP hernia surgery [2].
At present there is no definite evidence to demonstrate which mesh implantation and fixation method is best [3]. Studies have failed to demonstrate the influence of different mesh fixation techniques on post-operative outcomes and complications [4]. The primary purpose of this prospective study was to examine the outcomes and post-operative complications of TAPP without mesh fixation in inguinal hernia patients.
Materials and Methods
This study was conducted in post graduate department of surgery MMIMSR Ambala from March 2015 to June 2018. The study pattern was prospective with following study parameters:
Inclusion criteria
Patients with inguinal hernia and fit for general anaesthesia.
Exclusion criteria
1. Patients medically unfit for general anesthesia
2. Complicated hernia (obstructed hernia, strangulated hernia etc.)
3. Recurrent inguinal hernia
Technique
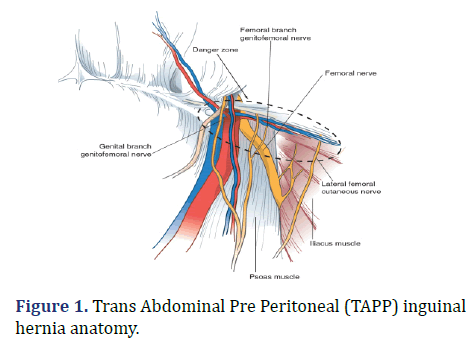
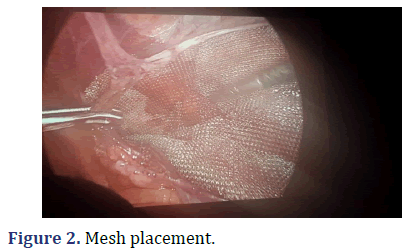
General anaesthesia was employed in all the cases. The operating table was placed in 15-30 degree Trendelenburg position. Right handed surgeon stood on the left side of the patient for right sided hernia while the camera assistant stood behind the operating surgeon. For a left inguinal hernia, mirror image position was adopted by the operating team. The monitor was placed at the right foot end level of the patient in left groin hernia and vice versa. Prophylactic antibiotic (inj ceftriaxone 1 gm IV stat) was given in all the cases. Peritoneal access was gained via infra umblical 10 mm port using Hasson’s open technique. Two additional ports 5 mm each were used for dissection and mesh placement. In unilateral hernia, the ipsilateral 5 mm port was made 2 cms above the umbilicus just lateral to the rectus, while the contralateral port was kept 2 cms below the umbilicus lateral to the rectus. In bilateral hernia, both 5 mm ports were made at the level of umbilicus lateral to the rectus. Peritoneal incision started at the level of Anterior Superior Iliac Spine avulsion (ASIS) till median umbilical fold in the space of Retzius. Medial dissection was performed first followed by the lateral dissection in avascular pre-peritoneal space with a combination of sharp and blunt dissection. Judicious use of diathermy was employed throughout the procedure to avoid post-operative seroma formation. Care was taken not to injure the cord structures in males. Cooper ligament was identified (Figure 1). In case of complete hernias, the hernial sac was divided after sufficient dissection to avoid injury to the cord structures and post-operative seroma formation. A 15 × 15 cm mesh tailored to 15 × 12 cms was introduced through 10 mm port and placed in pre-peritoneal space (Figure 2). The mesh was placed in such a way that at least half of it lays distal to the defect inferiorly, and the medial edge of the mesh crosses the midline by at least 2-3 cm. No tacks, sutures or sealants were used to fix the mesh. Hemostasis was ensured and the peritoneal incision closed with 2-0 running vicryl sutures. (Figure 3) fascial closure of 10 mm port was done with non-absorbable 1-0 prolene suture (Figures 1-3).
Results
A total of 43 patients were included in study (Table 1). All of them were males in the age group 17 to 65 years. 28 patients had indirect hernia, 13 had direct hernia while 2 patients had pantaloon hernia. Bilateral hernias were seen in 8 cases, all of them with direct sac. The mean operating time ranged 100 mins (90 to 120 minutes), starting from creation of camera port to complete peritoneal closure. Mean follow up period was 12 months (20 to 6 months). 19 patients had defect size between 1-1.5 cm while 24 patients had defect size between 1.5 to 3.0 cm. There was no death related to surgery (intraoperatively or within 30 days of operation). 2 patients (4.6%) developed minor umbilical port site infection which was managed conservatively with oral antibiotics and antiseptic dressings. 1 patient (2.3%) developed post-operative seroma formation which was managed successfully with observation and follow up. Inguinal pain described as dragging sensation or tightness in groin was observed in 19 patients (44.2%) post operatively, which disappeared as ambulation was encouraged. Only 1 patient (2.3%) reported chronic inguinal pain at 6 months of follow up. No recurrence was reported till the last follow up of each patient (Table 2).
| Summary characteristics | |
|---|---|
| Age | 60 yrs (17-65 years ) |
| M:F | 43:1 |
| Operating time | 90-120 min |
| Follow-up (time) | 12 months (20-6 months) |
| Parameter | Present study | Comparison |
|---|---|---|
| Recurrence | Nil | Nil Smith, et al [10] |
| Chronic groin pain | 2.3% | 1.67% Mohamed Abdelhamid, et al [12] |
Discussion
Ger in 1990 performed first laparoscopic hernia repair where he closed the defect with a simple mesh plug [5]. The concept of laparoscopic TAPP was revolutionized by Arregui and Dion [6]. Laparoscopic hernia surgery has several advantages over open Lichtenstein repair. It produces reduced post-operative, pain, wound infection, early return to normal activity and shorter hospital stay [7]. Since its evolution, mesh fixation in TAPP has remained a topic of debate. The need for fixing the mesh arises from the fear of increasing recurrence rates. Many studies have shown that laparoscopic inguinal hernia repair gives similar results in terms of recurrence as open hernia repair [8]. Recurrence may be attributed to technical difficulties and the use of inadequate mesh size and positioning [9]. Some studies suggest that in TAPP, mesh should be fixed prior to its fibrous incorporation so as to decrease the chances of recurrences [10]. A single randomized study in TAPP hernia by Smith [11] et al, showed no recurrences in over 250 patients without mesh fixation at a median follow-up of 16 months. Another large Multivariate analysis performed to identify the factors that have a significant impact on the recurrence rate in TAPP revealed that mesh fixation did not have any relevant impact on the recurrence rate regardless of the defect size [12].
Laparoscopic hernia has its own specific complications consequent to the use of mesh fixation devices. In a study conducted by Mohamed Abdelhamid, et al [13], 2 patients out of 120 developed post TAPP chronic groin pain. The pain is likely to be consequent to nerve entrapment during mesh fixation, however it may also occur due to nerve injury during dissection intraoperatively. Most surgeons currently performing laparoscopic hernia repair avoid mesh fixation during TEP, however the fear of recurrence compels most of them to tack or suture the mesh medially with cooper ligament and anterior abdominal wall during TAPP. Studies have shown that hernia recurrence bears little significance with mesh fixation while complications like inguinodynia can be minimized if mesh is not tacked or sutured during TAPP [11,13]. Avoiding stapling of the mesh helps in decreasing complications without affecting recurrence rates.
Seroma formation is another complication seen after laparoscopic hernia repair, more so with TEP [14]. The incidence is in the range of 5-25% [15]. Clinical factors associated with seroma formation include old age, large hernial defects, complete hernia, and the presence of a residual distal indirect sac. Our study finds no increased incidence of seroma formation post operatively.
Conclusion
To summarize, our rates of complications including seroma formation, recurrence and chronic groin pain are comparable to those described in the literature.
Our data supports the available evidence that repair without mesh fixation is possible with an acceptable rate of recurrence and a low rate of chronic groin pain. Hence there is no reason to routinely use a fixation device for laparoscopic TAPP hernia repair.
Conflict of Interest
The authors declare no conflict of interests.
Funding
None
References
- Wall ML, Cherian TH, Lotz JC. Laparoscopic Hernia Repair-The Best Option?. Acta Chir Belg 2008;108(2):186-191.
- MRC Laparoscopic Groin Hernia Trial Group. Laparoscopic versus open repair of groin hernia: A randomised comparison. Lancet 1999;354(9174):185-190.
- Schmedt CG, Sauerland S, Bittner R. Comparison of endoscopic procedures vs. Lichtenstein and other open mesh techniques for inguinal hernia repair: A meta-analysis of randomized controlled trials. Surg Endosc 2005;19:188-199.
- Mc Cormack K, Wake B, Perez J, Fraser C, Cook J, McIntosh E, et al. Laparoscopic surgery for inguinal hernia repair: systematic review of effectiveness and economic evaluation. Health Technol Assess 2005;9(14):1-203.
- Neugebauer E A M, Troidi H, Kum CK. The EAES Clinical Practice Guidelines on Laparoscopic Chole-cystectomy, Appendectomy and Hernia Repair. EAES Guidelines for Endoscopic Surgery, Springer, Berlin Heidelberg, 2006: 265-289.
- Mckernen JB. Laparoscopic preperitoneal prosthetic repair of inguinal hernias. Surg Rounds 1992;7:597-610.
- Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009;13:343-403.
- Köninger J, Redecke J, Butters M. Chronic pain after hernia repair: A randomized trial comparing Shouldice, Lichtenstein and TAPP. Langenbecks Arch Surg 2004;389:361-365.
- Watson A, Ziprin P, Chadwick S. TAPP repair for inguinal hernias–a new composite mesh technique. Ann R Coll Surg Engl 2006;88(7):678.
- Schwab R, Schumacher O, Junge K, Binnebösel M, Klinge U, Becker HP, et al. Biomechanical analyses of mesh fixation in TAPP and TEP hernia repair. Surg Endosc 2008;22:731-738.
- Smith AI, Royston CM, Sedman PC. Stapled and nonstapled laparoscopic transabdominal preperitoneal (TAPP) inguinal hernia repair: A prospective randomized trial. Surg Endosc 1999;13:804-806.
- Mayer F, Niebuhr H, Lechner M, Dinnewitzer A, Köhler G, Hukauf M, et al. When is mesh fixation in TAPP-repair of primary inguinal hernia repair necessary? The register-based analysis of 11,230 cases. Surg Endosc 2016;30:4363-4371.
- Abdelhamid M, Sadat AM, Abdelhaseeb AR, Nabil TM, Abdelbasset MS, Bechet AM, et al. Transabdominal Pre-Peritoneal Mesh for Inguinal Hernia Repair with External Fixation versus Mesh Stapling. Surg Sci 2013;4(11):516-519.
- Lau H, Lee F. Seroma following endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 2003;17:1773-1777.
- Kapiris SA, Brough WA, Royston CM, O’Boyle C, Sedman PC. Laparoscopic transabdominal preperitoneal (TAPP) hernia repair: A 7-year two-center experience in 3017 patients. Surg Endosc 2001;15:972-975.
Copyright: © 2023 The Authors. This is an open access article under the terms of the Creative Commons Attribution Non Commercial Share Alike 4.0 (https://creativecommons.org/licenses/by-nc-sa/4.0/). This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.